Thyroid
From Wikipedia, the free encyclopedia
| This article needs additional citations for verification. Please help improve this article by adding reliable references (ideally, using inline citations). Unsourced material may be challenged and removed. (June 2008) |
| Thyroid | |
|---|---|
| Endocrine system | |
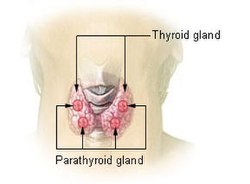
| Thyroid and parathyroid. | |
| Latin | glandula thyroidea |
| Gray's | subject #272 1269 |
| System | endocinal jubachina system |
| Artery | superior thyroid artery, inferior thyroid artery, thyreoidea ima,accessory thyroid arteries from oesophageal and tracheal branches |
| Vein | superior thyroid vein, middle thyroid vein, inferior thyroid vein,kocher's vein or 4th thyroid vein |
| Nerve | sympathetic system middle cervical ganglion, inferior cervical ganglion |
| Lymph | prelaryngeal, pretracheal, jugulo-diagastric groups of lymph nodes |
| Precursor | Thyroid diverticulum (an extension of endoderm into 2nd Branchial arch) |
| MeSH | Thyroid+Gland |
| Dorlands/Elsevier | Thyroid gland |
The thyroid is one of the largest endocrine glands in the body. This gland is found in the neck inferior to (below) the thyroid cartilage (also known as the Adam's apple in men) and at approximately the same level as the cricoid cartilage. The thyroid controls how quickly the body burns energy, makes proteins, and how sensitive the body should be to other hormones.
The thyroid participates in these processes by producing thyroid hormones, principally thyroxine (T4) and triiodothyronine (T3). These hormones regulate the rate of metabolism and affect the growth and rate of function of many other systems in the body. Iodine is an essential component of both T3 and T4. The thyroid also produces the hormone calcitonin, which plays a role in calcium homeostasis.
The thyroid is controlled by the hypothalamus and pituitary. The gland gets its name from the Greek word for "shield", after the shape of the related thyroid cartilage. Hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) are the most common problems of the thyroid gland.
Contents |
[edit] Anatomy
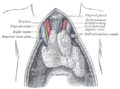
The thyroid gland is butterfly-shaped organ and is composed of two cone-like lobes or wings: lobus dexter (right lobe) and lobus sinister (left lobe), connected with the isthmus. The organ is situated on the anterior side of the neck, lying against and around the larynx and trachea, reaching posteriorly the oesophagus and carotid sheath. It starts cranially at the oblique line on the thyroid cartilage (just below the laryngeal prominence or Adam's apple) and extends inferiorly to the fourth to sixth tracheal ring[citation needed]. It is difficult to demarcate the gland's upper and lower border with vertebral levels as it moves position in relation to these during swallowing.
The thyroid gland is covered by a fibrous sheath, the capsula glandulae thyroidea, composed of an internal and external layer. The external layer is anteriorly continuous with the lamina pretrachealis fasciae cervicalis and posteriorolaterally continuous with the carotid sheath. The gland is covered anteriorly with infrahyoid muscles and laterally with the sternocleidomastoid muscle. Posteriorly, the gland is fixed to the cricoid and tracheal cartilage and cricopharyngeus muscle by a thickening of the fascia to form the posterior suspensory ligament of Berry[1][2]. In variable extent, Lalouette's Pyramid, a pyramidal extension of the thyroid lobe, is present at the most anterior side of the lobe. In this region the recurrent laryngeal nerve and the inferior thyroid artery pass next to or in the ligament and tubercle. Between the two layers of the capsule and on the posterior side of the lobes there are on each side two parathyroid glands.
The thyroid isthmus is variable in presence and size, and can encompass a cranially extending pyramid lobe (lobus pyramidalis or processus pyramidalis), remnant of the thyroglossal duct. The thyroid is one of the larger endocrine glands, weighing 2-3 grams in neonates and 18-60 grams in adults, and is increased in pregnancy[citation needed].
The thyroid is supplied with arterial blood from the superior thyroid artery, a branch of the external carotid artery, and the inferior thyroid artery, a branch of the thyrocervical trunk, and sometimes by the thyroid ima artery, branching directly from the aortic arch. The venous blood is drained via superior thyroid veins, draining in the internal jugular vein, and via inferior thyroid veins, draining via the plexus thyroideus impar in the left brachiocephalic vein. Lymphatic drainage passes frequently the lateral deep cervical lymph nodes and the pre- and parathracheal lymph nodes. The gland is supplied by sympathetic nerve input from the superior cervical ganglion and the cervicothoracic ganglion of the sympathetic trunk[citation needed], and by parasympathetic nerve input from the superior laryngeal nerve and the recurrent laryngeal nerve.
[edit] Embryological development
| This section does not cite any references or sources. Please help improve this article by adding citations to reliable sources (ideally, using inline citations). Unsourced material may be challenged and removed. (January 2008) |
In the fetus, at 3-4 weeks of gestation, the thyroid gland appears as an epithelial proliferation in the floor of the pharynx at the base of the tongue between the tuberculum impar and the copula linguae at a point latter indicated by the foramen cecum. Subsequently the thyroid descends in front of the pharyngeal gut as a bilobed diverticulum through the thyroglossal duct. Over the next few weeks, it migrates to the base of the neck. During migration, the thyroid remains connected to the tongue by a narrow canal, the thyroglossal duct. The fetus starts making its own thyroid-stimulating hormone (TSH) by week 8, and the follicles of the thyroid begin to make colloid and thyroxine by the 10th week.
[edit] Histology
| This section does not cite any references or sources. Please help improve this article by adding citations to reliable sources (ideally, using inline citations). Unsourced material may be challenged and removed. (January 2008) |
At the microscopic level, there are three primary features of the thyroid:
| Feature | Description |
| Follicles | The thyroid is composed of spherical follicles that selectively absorb iodine (as iodide ions, I-) from the blood for production of thyroid hormones. Twenty-five percent of all the body's iodide ions are in the thyroid gland. Inside the follicles, colloid serve as a reservoir of materials for thyroid hormone production and, to a lesser extent, act as a reservoir for the hormones themselves. Colloid is rich in a protein called thyroglobulin. |
| Thyroid epithelial cells (or "follicular cells") |
The follicles are surrounded by a single layer of thyroid epithelial cells, which secrete T3 and T4. When the gland is not secreting T3/T4 (inactive), the epithelial cells range from low columnar to cuboidal cells. When active, the epithelial cells become tall columnar cells. |
| Parafollicular cells (or "C cells") |
Scattered among follicular cells and in spaces between the spherical follicles are another type of thyroid cell, parafollicular cells, which secrete calcitonin. |
[edit] Physiology
The primary function of the thyroid is production of the hormones thyroxine (T4), triiodothyronine (T3), and calcitonin. Up to 80% of the T4 is converted to T3 by peripheral organs such as the liver, kidney and spleen. T3 is about ten times more active than T4.[3]
[edit] T3 and T4 production and action
Thyroxine (T4) is synthesised by the follicular cells from free tyrosine and on the tyrosine residues of the protein called thyroglobulin (TG). Iodine is captured with the "iodine trap" by the hydrogen peroxide generated by the enzyme thyroid peroxidase (TPO)[4] and linked to the 3' and 5' sites of the benzene ring of the tyrosine residues on TG, and on free tyrosine. Upon stimulation by the thyroid-stimulating hormone (TSH), the follicular cells reabsorb TG and proteolytically cleave the iodinated tyrosines from TG, forming T4 and T3 (in T3, one iodine is absent compared to T4), and releasing them into the blood. Deiodinase enzymes convert T4 to T3.[5] Thyroid hormone that is secreted from the gland is about 90% T4 and about 10% T3.[3]
Cells of the brain are a major target for the thyroid hormones T3 and T4. Thyroid hormones play a particularly crucial role in brain maturation during fetal development.[6] A transport protein (OATP1C1) has been identified that seems to be important for T4 transport across the blood brain barrier.[7] A second transport protein (MCT8) is important for T3 transport across brain cell membranes.[7]
In the blood, T4 and T3 are partially bound to thyroxine-binding globulin, transthyretin and albumin. Only a very small fraction of the circulating hormone is free (unbound) - T4 0.03% and T3 0.3%. Only the free fraction has hormonal activity. As with the steroid hormones and retinoic acid, thyroid hormones cross the cell membrane and bind to intracellular receptors (α1, α2, β1 and β2), which act alone, in pairs or together with the retinoid X-receptor as transcription factors to modulate DNA transcription[1].
[edit] T3 and T4 regulation
The production of thyroxine and triiodothyronine is regulated by thyroid-stimulating hormone (TSH), released by the anterior pituitary (that is in turn released as a result of TRH release by the hypothalamus). The thyroid and thyrotropes form a negative feedback loop: TSH production is suppressed when the T4 levels are high, and vice versa. The TSH production itself is modulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus and secreted at an increased rate in situations such as cold (in which an accelerated metabolism would generate more heat). TSH production is blunted by somatostatin (SRIH), rising levels of glucocorticoids and sex hormones (estrogen and testosterone), and excessively high blood iodide concentration.
[edit] Calcitonin
An additional hormone produced by the thyroid contributes to the regulation of blood calcium levels. Parafollicular cells produce calcitonin in response to hypercalcemia. Calcitonin stimulates movement of calcium into bone, in opposition to the effects of parathyroid hormone (PTH). However, calcitonin seems far less essential than PTH, as calcium metabolism remains clinically normal after removal of the thyroid, but not the parathyroids.
[edit] Significance of iodine
In areas of the world where iodine (essential for the production of thyroxine, which contains four iodine atoms) is lacking in the diet, the thyroid gland can be considerably enlarged, resulting in the swollen necks of endemic goitre.
Thyroxine is critical to the regulation of metabolism and growth throughout the animal kingdom. Among amphibians, for example, administering a thyroid-blocking agent such as propylthiouracil (PTU) can prevent tadpoles from metamorphosing into frogs; conversely, administering thyroxine will trigger metamorphosis.
In humans, children born with thyroid hormone deficiency will have physical growth and development problems, and brain development can also be severely impaired, in the condition referred to as cretinism. Newborn children in many developed countries are now routinely tested for thyroid hormone deficiency as part of newborn screening by analysis of a drop of blood. Children with thyroid hormone deficiency are treated by supplementation with synthetic thyroxine, which enables them to grow and develop normally.
Because of the thyroid's selective uptake and concentration of what is a fairly rare element, it is sensitive to the effects of various radioactive isotopes of iodine produced by nuclear fission. In the event of large accidental releases of such material into the environment, the uptake of radioactive iodine isotopes by the thyroid can, in theory, be blocked by saturating the uptake mechanism with a large surplus of non-radioactive iodine, taken in the form of potassium iodide tablets. While biological researchers making compounds labelled with iodine isotopes do this, in the wider world such preventive measures are usually not stockpiled before an accident, nor are they distributed adequately afterward. One consequence of the Chernobyl disaster was an increase in thyroid cancers in children in the years following the accident.[8]
The use of iodised salt is an efficient way to add iodine to the diet. It has eliminated endemic cretinism in most developed countries, and some governments have made the iodination of flour or salt mandatory. Potassium iodide and Sodium iodide are the most active forms of supplemental iodine.
Contradictory, recent studies on some populations are showing that excess of iodine could be related to the raise of autoimmune disease driving to permanent Hypothyroidism.[9]. Some governments are reviewing the quantity of iodine added to salt using local salt consumption data.[citation needed]
[edit] History
There are several findings that evidence a great interest for thyroid disorders just in the Medieval Medical School of Salerno (XII Century). Rogerius Salernitanus, the Salernitan surgeon and author of "Post mundi fabricam" (around 1180) was considered at that time the surgical text par excellence all over Europe. In the chapter "De bocio" of his magnum opus he describes several pharmacological and surgical cures, some of which nowadays are reappraised quite scientifically effective.[10]
In modern times, the thyroid was first identified by the anatomist Thomas Wharton (whose name is also eponymised in Wharton's duct of the submandibular gland) in 1656.[11]
Thyroid hormone (or thyroxin) was identified only in the 19th century.
[edit] Additional images
|
Section of thyroid gland of sheep. X 160. |
|||
[edit] See also
[edit] References
- ^ Yalçin B., Ozan H. (February 2006). "Detailed investigation of the relationship between the inferior laryngeal nerve including laryngeal branches and ligament of Berry". Journal of the American College of Surgeons 202 (2): 291–6. doi:. PMID 16427555.
- ^ Lemaire, David (2005-05-27), eMedicine - Thyroid anatomy, http://www.emedicine.com/ent/topic532.htm, retrieved on 2008-01-19
- ^ a b The thyroid gland in Endocrinology: An Integrated Approach by Stephen Nussey and Saffron Whitehead (2001) Published by BIOS Scientific Publishers Ltd. ISBN 1-85996-252-1 .
- ^ Ekholm R, Bjorkman U (1997). "Glutathione peroxidase degrades intracellular hydrogen peroxide and thereby inhibits intracellular protein iodination in thyroid epithelium". Endocrinology 138 (7): 2871–2878. doi:. PMID 9202230.
- ^ Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR (2002). "Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases". Endocr Rev 23 (1): 38–89. doi:. PMID 11844744.
- ^ Kester MH, Martinez de Mena R, Obregon MJ, Marinkovic D, Howatson A, Visser TJ, Hume R, Morreale de Escobar G (2004). "Iodothyronine levels in the human developing brain: major regulatory roles of iodothyronine deiodinases in different areas". J Clin Endocrinol Metab 89 (7): 3117–3128. doi:. PMID 15240580.
- ^ a b Jansen J, Friesema ECH, Milici C, Visser TJ (2005). Thyroid hormone transporters in health and disease. Thyroid 15;757-768. PMID 16131319.
- ^ BBC NEWS | Science/Nature | Chernobyl children show DNA changes
- ^ Patrick L (June 2008). "Iodine: deficiency and therapeutic considerations" (PDF). Altern Med Rev 13 (2): 116–27. PMID 18590348. http://www.thorne.com/altmedrev/.fulltext/13/2/116.pdf.
- ^ Bifulco M, Cavallo P (2007). "Thyroidology in the medieval medical school of salerno". Thyroid 17 (1): 39–40. doi:. PMID 17274747.
- ^ Thomas Wharton at Who Named It?
[edit] External links
- American Thyroid Association (Thyroid Information and professional organization)
- Histology at KUMC epithel-epith03 "Thyroid Gland"
- New Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer from the American Thyroid Association Taskforce.
- Thyroid Disease Manager (free online textbook)
- Thyroid Disease (Nuclear Medicine Information)
- The Thyroid Foundation of America (Education about Thyroid Disease)
|
|||||||||||||||||||||||||||