Heart
From Wikipedia, the free encyclopedia
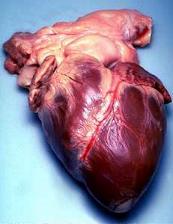
The heart is a muscular organ in all vertebrates responsible for pumping blood through the blood vessels by repeated, rhythmic contractions, or a similar structure in annelids, mollusks, and arthropods. The term cardiac (as in cardiology) means "related to the heart" and comes from the Greek καρδιά, kardia, for "heart."
The heart of a vertebrate is composed of cardiac muscle, an involuntary muscle tissue which is found only within this organ. The average human heart, beating at 72 beats per minute, will beat approximately 2.5 billion times during a lifetime (about 66 years). It weighs on average 250 g to 300 g in females and 300 g to 350 g in males.[1]
Contents |
[edit] Early development
The reptilian heart is derived from embryonic mesoderm germ-layer cells that differentiate after gastrulation into mesothelium, endothelium, and myocardium. Mesothelial pericardium forms the inner lining of the heart. The outer lining of the heart, lymphatic and blood vessels develop from endothelium. Myocardium develops into heart muscle.[2]
From splachnopleuric mesoderm tissue, the cardiogenic plate develops cranially and laterally to the neural plate. In the cardiogenic plate, two separate angiogenic cell clusters form on either side of the embryo. Each cell cluster coalesces to form an endocardial tube continuous with a dorsal aorta and a vitteloumbilical vein. As embryonic tissue continues to fold, the two endocardial tubes are pushed into the thoracic cavity and begin to fuse together and are completely fused at approximately 21 days.[3]

The human embryonic heart begins beating around 23 days after conception, or five weeks after the last normal menstrual period (LMP), which is the date normally used to date pregnancy. It is unknown how blood in the human embryo circulates for the first 21 days in the absence of a functioning heart. The human heart begins beating at a rate near the mother’s, about 75-80 beats per minute (BPM).
The embryonic heart rate (EHR) then accelerates by 150 for the first month of beating, peaking at 265-285 BPM during the early 7th week, (early 9th week after the LMP). This acceleration is approximately 3.3 BPM per day, or about 10 BPM every three days, an increase of 100 BPM in the first month.[4] At about 9.1 weeks after the LMP, it decelerates to about 152 BPM (+/-25 BPM) during the 15th week after the LMP. After the 15th week the deceleration slows reaching an average rate of about 145 (+/-25 BPM) BPM at term. The regression formula which describes this acceleration before the embryo reaches 25 mm in crown-rump length or 9.2 LMP weeks is Age in days = EHR(0.3)+6.
There is no difference in male and female heart rates before birth, as found by Dr. Dylan Angiolillo in 1995.[5]
[edit] Structure
The structure of the heart varies among the different branches of the animal kingdom. (See Circulatory system.) Cephalopods have two "gill hearts" and one "systemic heart". Fish have a two-chambered heart that pumps the blood to the gills and from there it goes on to the rest of the body. In amphibians and most reptiles, a double circulatory system is used, but the heart is not always completely separated into two pumps. Amphibians have a three-chambered heart.

-A point 9 cm to the left of the midsternal line (apex of the heart)
-The seventh right sternocostal articulation
-The upper border of the third right costal cartilage 1 cm from the right sternal line
-The lower border of the second left costal cartilage 2.5 cm from the left lateral sternal line.[6]
Birds and mammals show complete separation of the heart into two pumps, for a total of four heart chambers; it is thought that the four-chambered heart of birds evolved independently from that of mammals.
In the human body, the heart is usually situated in the middle of the thorax with the largest part of the heart slightly offset to the left (although sometimes it is on the right, see dextrocardia), underneath the breastbone. The heart is usually felt to be on the left side because the left heart (left ventricle) is stronger (it pumps to all body parts). The left lung is smaller than the right lung because the heart occupies more of the left hemithorax. The heart is fed by the coronary circulation and enclosed by a sac known as the pericardium and is surrounded by the lungs. The pericardium comprises two parts: the fibrous pericardium, made of dense fibrous connective tissue; and a double membrane structure (parietal and visceral pericardium) containing a serous fluid to reduce friction during heart contractions. The heart is located in the mediastinum, the central subdivision of the thoracic cavity. The mediastinum also contains other structures, such as the oesophagus and trachea, and is flanked on either side by the right and left pulmonary cavities, which house the lungs. [7]
The apex is the blunt point situated in an inferior (pointing down and left) direction. A stethoscope can be placed directly over the apex so that the beats can be counted. It is located posterior to the 5th intercostal space just medial of the left mid-clavicular line. In normal adults, the mass of the heart is 250-350 g (9-12 oz), or about twice the size of a clenched fist (it is about the size of a clenched fist in children), but extremely diseased hearts can be up to 1000 g (2 lb) in mass due to hypertrophy. It consists of four chambers, the two upper atria (singular: atrium ) and the two lower ventricles.
[edit] Functioning
| This section does not cite any references or sources. Please help improve this article by adding citations to reliable sources (ideally, using inline citations). Unsourced material may be challenged and removed. (June 2008) |
In mammals, the function of the right side of the heart (see right heart) is to collect de-oxygenated blood, in the right atrium, from the body (via superior and inferior vena cavae) and pump it, via the right ventricle, into the lungs (pulmonary circulation) so that carbon dioxide can be dropped off and oxygen picked up (gas exchange). This happens through the passive process of diffusion. The left side (see left heart) collects oxygenated blood from the lungs into the left atrium. From the left atrium the blood moves to the left ventricle which pumps it out to the body (via the aorta). On both sides, the lower ventricles are thicker and stronger than the upper atria. The muscle wall surrounding the left ventricle is thicker than the wall surrounding the right ventricle due to the higher force needed to pump the blood through the systemic circulation.
Starting in the right atrium, the blood flows through the tricuspid valve to the right ventricle. Here it is pumped out the pulmonary semilunar valve and travels through the pulmonary artery to the lungs. From there, blood flows back through the pulmonary vein to the left atrium. It then travels through the mitral valve to the left ventricle, from where it is pumped through the aortic semilunar valve to the aorta. The aorta forks, and the blood is divided between major arteries which supply the upper and lower body. The blood travels in the arteries to the smaller arterioles, then finally to the tiny capillaries which feed each cell. The (relatively) deoxygenated blood then travels to the venules, which coalesce into veins, then to the inferior and superior venae cavae and finally back to the right atrium where the process began.
The heart is effectively a syncytium, a meshwork of cardiac muscle cells interconnected by contiguous cytoplasmic bridges. This relates to electrical stimulation of one cell spreading to neighboring cells.
Some cardiac cells are self-excitable, contracting without any signal from the nervous system, even if removed from the heart and placed in culture. Each of these cells has its own intrinsic contraction rhythm. A region of the human heart called the sinoatrial node SA node, or pacemaker, sets the rate and timing at which all cardiac muscle cells contract. The SA node generates electrical impulses, much like those produced by nerve cells. Because cardiac muscle cells are electrically coupled by intercalated disks between adjacent cells, impulses from the SA node spread rapidly through the walls of the artria, causing both artria to contract in unison. The impulses also pass to another region of specialized cardiac muscle tissue, a relay point called the atrioventricular (AV) node, located in the wall between the right artrium and the right ventricle. Here, the impulses are delayed for about 0.1s before spreading to the walls of the ventricle. The delay ensures that the artria empty completely before the ventricles contract. Specialized muscle fibers called Purkinje fibers then conduct the signals to the apex of the heart along and throughout the ventricular walls. The Purkinje fibres form conducting pathways called bundle branches. The impulses generated during the heart cycle produce electrical currents, which are conducted through body fluids to the skin, where thery can be detected by electrodes and recorded as an electrocardiogram (ECG or EKG).[8]
[edit] First aid
| This section does not cite any references or sources. Please help improve this article by adding citations to reliable sources (ideally, using inline citations). Unsourced material may be challenged and removed. (June 2008) |
The heart is one of the critical organs of an animal's body, as it pumps oxygenated blood to feed the body's biological functions. The cessation of the heartbeat, referred to as cardiac arrest, is a critical emergency. Without intervention, death can occur within minutes of cardiac arrest since the brain requires a continuous supply of oxygen and cannot survive for long if that supply is cut off.
If a person is encountered in cardiac arrest, cardiopulmonary resuscitation (CPR) should be started and help called. Use of a defibrillator is preferred, if available, to attempt to restore a normal heartbeat; many public areas have portable defibrillators available for such emergencies. Usually, if there is enough time, the person can be rushed to the hospital where he or she will be resuscitated in the Emergency Department.
Electrical innervation of the heart in health is supplied by two closely intertwined mechanisms. The first mechanism is well demonstrated in electrical coil systole (interpreted by the electrocardiogram as QRS) as an individualized myocardial electrical tree initiated by the sinoatrial node. Secondary diastolic electrical control is posited to represent autonomic recoil control from the vagus nerve and cardiac branches and the thoracic ganglia.
[edit] History of discoveries
| This section does not cite any references or sources. Please help improve this article by adding citations to reliable sources (ideally, using inline citations). Unsourced material may be challenged and removed. (June 2008) |
The valves of the heart were discovered by a physician of the Hippocratean school around the 4th century BC. However, their function was not properly understood then. Because blood pools in the veins after death, arteries look empty. Ancient anatomists assumed they were filled with air and that they were for transport of air.
Philosophers distinguished veins from arteries but thought that the pulse was a property of arteries themselves. Erasistratos observed that arteries that were cut during life bleed. He ascribed the fact to the phenomenon that air escaping from an artery is replaced with blood that entered by very small vessels between veins and arteries. Thus he apparently postulated capillaries but with reversed flow of blood.
The 2nd century AD, Greek physician Galenos (Galen) knew that blood vessels carried blood and identified venous (dark red) and arterial (brighter and thinner) blood, each with distinct and separate functions. Growth and energy were derived from venous blood created in the liver from chyle, while arterial blood gave vitality by containing pneuma (air) and originated in the heart. Blood flowed from both creating organs to all parts of the body where it was consumed and there was no return of blood to the heart or liver. The heart did not pump blood around, the heart's motion sucked blood in during diastole and the blood moved by the pulsation of the arteries themselves.
Galen believed that the arterial blood was created by venous blood passing from the left ventricle to the right by passing through 'pores' in the inter ventricular septum, air passed from the lungs via the pulmonary artery to the left side of the heart. As the arterial blood was created 'sooty' vapors were created and passed to the lungs also via the pulmonary artery to be exhaled.
The modern understanding of the anatomy of the heart is due to cardiologist Dr. Francisco Torrent-Guasp, who in 1997 published his theory on the physiology and function of the heart, after more than 40 years of study. Doctor Torrent's model describes the heart as a single band of muscle starting at the pulmonary artery and ending below the aorta exit. This band wraps itself into a double helical coil that bounds both ventricular cavities with a wall that separates them. His model also describes how this band progressively contracts leading to ejection and suction of the blood. This model has been a major achievement, since it was widely believed until then that blood blue entered the left ventricle passively. It has also led to the introduction of several new surgical techniques.
[edit] Healthy heart
Obesity, high blood pressure and high cholesterol can increase the risk of developing heart disease. However, fully half the amount of heart attacks occur in people with normal cholesterol levels. Inflammation is now considered an important consideration more so than total cholesterol levels.[citation needed] Heart disease is a major cause of death (and the number one cause of death in the Western World).
Note also suggestions that drinking certain types of red wine in moderation can reduce the risk of heart disease. This is widely used as a reason for why people in France can apparently enjoy such rich food, and yet suffer relatively fewer heart problems. Of course one must also consider other factors such as lifestyle and overall health (mental and social as well as physical).[9][10][11][12]
[edit] Food use
| This section does not cite any references or sources. Please help improve this article by adding citations to reliable sources (ideally, using inline citations). Unsourced material may be challenged and removed. (June 2008) |
The hearts of cattle, sheep, pigs, chickens and certain fowl are consumed in many countries. They are counted among offal, but being a muscle, the taste of heart is like regular meat. It resembles venison in structure and taste.
[edit] See also
[edit] References
- ^ Kumar, Abbas, Fausto: Robbins and Cotran Pathologic Basis of Disease, 7th Ed. p. 556
- ^ Animal Tissues
- ^ Main Frame Heart Development>
- ^ OBGYN.net "Embryonic Heart Rates Compared in Assisted and Non-Assisted Pregnancies"
- ^ Terry J. DuBose http://www.obgyn.net/english/pubs/features/dubose/ehr-age.htm Sex, Heart Rate and Age]
- ^ Gray's Anatomy of the Human Body - 6. Surface Markings of the Thorax
- ^ Maton, Anthea; Jean Hopkins, Charles William McLaughlin, Susan Johnson, Maryanna Quon Warner, David LaHart, Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey: Prentice Hall. ISBN 0-13-981176-1. OCLC 32308337.
- ^ Campbell, Reece-Biology, 7th Ed. p.873,874
- ^ "Eating for a healthy heart". MedicineWeb. http://www.medicineweb.com/nutrition-/eating-for-a-healthy-heart. Retrieved on 2009-03-31.
- ^ Division of Vital Statistics; Arialdi M. Miniño, M.P.H., Melonie P. Heron, Ph.D., Sherry L. Murphy, B.S., Kenneth D. Kochanek, M.A. (2007-08-21). "Deaths: Final data for 2004" (PDF). National Vital Statistics Reports (United States: Center for Disease Control) 55 (19): 7. http://www.cdc.gov/nchs/data/nvsr/nvsr55/nvsr55_19.pdf. Retrieved on 2007-12-30.
- ^ White House News, American Heart Month, 2007, http://www.whitehouse.gov/news/releases/2007/02/20070201-2.html, retrieved on 2007-07-16
- ^ National Statistics Press Release 25 May 2006
[edit] External links
| Look up heart in Wiktionary, the free dictionary. |
| Wikimedia Commons has media related to: Heart |
- Heart contraction and blood flow (animation)
- Heart Disease
- eMedicine: Surgical anatomy of the heart
- Interactive 3D heart This realistic heart can be rotated, and all its components can be studied from any angle.
|
||||||||||||||||||||
|
|||||||||||