Statin
From Wikipedia, the free encyclopedia

The statins (or HMG-CoA reductase inhibitors) are a class of drugs that lower cholesterol levels in people with or at risk of cardiovascular disease.
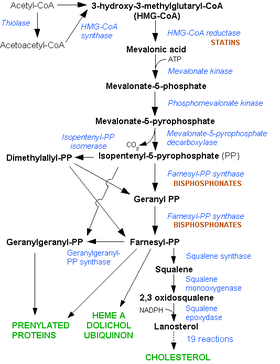
They lower cholesterol by inhibiting the enzyme HMG-CoA reductase, which is the rate-limiting enzyme of the mevalonate pathway of cholesterol synthesis. Inhibition of this enzyme in the liver results in decreased cholesterol synthesis as well as increased synthesis of LDL receptors, resulting in an increased clearance of low-density lipoprotein (LDL) from the bloodstream. The first results can be seen after one week of use and the effect is maximal after four to six weeks.
Contents |
[edit] History
Akira Endo and Masao Kuroda of Tokyo, Japan commenced research into inhibitors of HMG-CoA reductase in 1971 (Endo 1992). This team reasoned that certain microorganisms may produce inhibitors of the enzyme to defend themselves against other organisms, as mevalonate is a precursor of many substances required by organisms for the maintenance of their cell wall (ergosterol) or cytoskeleton (isoprenoids).[1]
The first agent isolated was mevastatin (ML-236B), a molecule produced by Penicillium citrinum. The pharmaceutical company Merck & Co. showed an interest in the Japanese research in 1976, and isolated lovastatin (mevinolin, MK803), the first commercially marketed statin, from the mold Aspergillus terreus. Dr Endo was awarded the 2006 Japan Prize for his work on the development of statins, and the Clinical Medical Research Award from the Lasker Foundation in 2008.
[edit] Mechanism of action
Statins act by inhibiting the enzyme HMG-CoA reductase, the enzyme controlling the first committed step of sterol (cholesterol) synthesis, in the liver. Because statins are similar to HMG-CoA on a molecular level they take the place of HMG-CoA in the enzyme and reduce the rate by which it is able to produce mevalonate, the next molecule in the cascade that eventually produces cholesterol, as well as a number of other compounds.
Inside the liver cell, other enzymes of the protease class sense the decreased level of cholesterol produced. In response, they cleave a protein called "membrane-bound sterol regulatory element binding protein", which then responds by migrating to the nucleus to increase production of various other proteins and enzymes, including the LDL receptor. The LDL receptor then relocates to the cell membrane of the liver cell, and binds to passing low density lipoprotein and very low density lipoprotein particles (both containing cholesterol in the undesired form). LDL and VLDL enter the liver and are digested.
[edit] Indications and uses
Statins, the most potent cholesterol-lowering agents available, lower LDL cholesterol (so-called "bad cholesterol") by 1.8 mmol/l. This translates in a 60% decrease in the number of cardiac events (heart attack, sudden cardiac death), and a 17% reduced risk of stroke.[2] They have less effect than the fibrates or niacin in reducing triglycerides and raising HDL-cholesterol ("good cholesterol"). Professional guidelines generally require that the patient has tried a cholesterol-lowering diet before statin use is considered; statins or other pharmacologic agents may then be recommended for patients who do not meet their lipid-lowering goals through diet and lifestyle approaches.
The indications for the prescription of statins have broadened over the years. Initial studies, such as the Scandinavian Simvastatin Survival Study (4S), supported the use of statins in secondary prevention for cardiovascular disease, or as primary prevention only when the risk for cardiovascular disease was significantly raised (as indicated by the Framingham risk score).[3] Indications were broadened considerably by studies such as the Heart Protection Study (HPS), which showed preventative effects of statin use in specific risk groups, such as diabetics. The ASTEROID trial, published in 2006, using only a statin at high dose, achieved lower than usual target calculated LDL values and showed disease regression within the coronary arteries using intravascular ultrasonography.[4]
Based on clinical trials, the National Cholesterol Education Program guidelines, and the increasing focus on aggressively lowering LDL-cholesterol, the statins continue to play an important role in both the primary and secondary prevention of coronary heart disease, myocardial infarction, stroke and peripheral artery disease.
Research continues into other areas where statins also appear to have a favorable effect: inflammation, dementia,[5] cancer,[6] nuclear cataracts,[7] and hypertension.[8]
[edit] Members
[edit] Fermentation-derived and synthetic
The statins are divided into two groups: fermentation-derived and synthetic.
The statins include, in alphabetical order (brand names vary in different countries):
| Statin | Brand name | Derivation |
| Atorvastatin | Lipitor, Torvast | Synthetic |
| Cerivastatin | Lipobay, Baycol. (Withdrawn from the market in August, 2001 due to risk of serious Rhabdomyolysis) | Synthetic |
| Fluvastatin | Lescol, Lescol XL | Synthetic |
| Lovastatin | Mevacor, Altocor, Altoprev | Fermentation-derived |
| Mevastatin | - | Naturally-occurring compound. Found in red yeast rice. |
| Pitavastatin | Livalo, Pitava | Synthetic |
| Pravastatin | Pravachol, Selektine, Lipostat | Fermentation-derived |
| Rosuvastatin | Crestor | Synthetic |
| Simvastatin | Zocor, Lipex | Fermentation-derived. (Simvastatin is a synthetic derivate of a fermentation product) |
| Simvastatin+Ezetimibe | Vytorin | Combination therapy |
| Lovastatin+Niacin extended-release | Advicor | Combination therapy |
| Atorvastatin+Amlodipine Besylate | Caduet | Combination therapy - Cholesterol+Blood Pressure |
| Simvastatin+Niacin extended-release | Simcor | Combination therapy |
LDL-lowering potency varies between agents. Cerivastatin is the most potent, followed by (in order of decreasing potency) atorvastatin, rosuvastatin, simvastatin, lovastatin, pravastatin, and fluvastatin.[9] The relative potency of pitavastatin has not yet been fully established.
[edit] Comparative effectiveness
No large scale comparison exists that examines the relative effectiveness of the various statins against one another for preventing hard cardiovascular outcomes, such as death or myocardial infarction.
An independent analysis has been done to compare atorvastatin, pravastatin and simvastatin, based on their effectiveness against placebos. It found that, at commonly prescribed doses, there are no statistically significant differences in reducing cardiovascular morbidity and mortality.[10] The CURVES study, which compared the efficacy of different doses of atorvastatin, simvastatin, pravastatin, lovastatin, and fluvastatin for reducing LDL and total cholesterol in patients with hypercholesterolemia, found that atorvastatin was more effective without increasing adverse events.[11]
[edit] Cost effectiveness
Statins vary in cost from $32 to $150 a month. Consumer Reports recommends generic lovastatin, pravastatin, and simvastatin as cost-efficient "Best Buy" alternatives to more expensive branded drugs, for those in whom it is suitable. Costs can be further reduced by splitting tablets in half. [12]
[edit] Safety
[edit] Adverse effects
Statins are generally well-tolerated and have only two major side effects that occur relatively rarely: raised liver enzymes and skeletal muscle pain and/or damage.
While some patients on statin therapy report myalgias, muscle cramps, or far less-frequent gastrointestinal or other symptoms, similar symptoms are also reported with placebo use in all the large statin safety/efficacy trials and usually resolve, either on their own or on temporarily lowering/stopping the dose. Liver enzyme derangements may also occur, typically in about 0.5%,[citation needed] are also seen at similar rates with placebo use and repeated enzyme testing, and generally return to normal either without discontinuance over time or after briefly discontinuing the drug. Multiple other side-effects occur rarely; typically also at similar rates with only placebo in the large statin safety/efficacy trials.
More serious but rare reactions include myositis and myopathy, with the potential for rhabdomyolysis (the pathological breakdown of skeletal muscle) leading to acute renal failure. Coenzyme Q10 (ubiquinone) levels are decreased in statin use;[13] Q10 supplements are sometimes used to treat statin-associated myopathy, though evidence of their effectiveness is currently lacking.[14] A common variation in the SLCO1B1 gene, which participates in the absorption of statins, has been shown to significantly increase the risk of myopathy.[15]
Graham etal (2004) reviewed records of over 250,000 patients treated from 1998 to 1991 with the statin drugs atorvastatin, cerivastatin, fluvastatin, lovastatin, pravastatin, and simvastatin.[16] The incidence of rhabdomyolyis was 0.44 per 10,000 patients treated with statins other than cerivastatin. However, the risk was over ten fold greater if cerivastatin was used, or if the standard statins (atorvastatin, fluvastatin, lovastatin, pravastatin, simvastatin) were combined with fibrate (fenofibrate or gemfibrozil) treatment. Cerivastatin was withdrawn by its manufacturer in 2001.
All commonly used statins show somewhat similar results, however the newer statins, characterized by longer pharmacological half-lives and more cellular specificity, have had a better ratio of efficacy to lower adverse effect rates. The risk of myopathy is lowest with pravastatin and fluvastatin probably because they are more hydrophillic and as a result have less muscle penetration. Lovastatin induces the expression of gene atrogin-1, which is believed to be responsible in promoting muscle fiber damage.[17]
Despite initial concerns that statins might increase the risk of cancer, various studies concluded later that statins have no influence on cancer risk (including the heart protection study and a 2006 meta-analysis[18]). Indeed, a 2005 trial showed that patients taking statins for over 5 years reduced their risk of colorectal cancer by 50%; this effect was not exhibited by fibrates. The trialists warn that the number needed to treat would approximate 5000, making statins unlikely tools for primary prevention.[19] However, in a recent meta-analysis of 23 statin treatment arms with 309,506 person-years of follow-up, there was an inverse relationship between achieved LDL-cholesterol levels and rates of newly diagnosed cancer that the authors claim requires further investigation.[20]
[edit] Drug interactions
Combining any statin with a fibrate, another category of lipid-lowering drugs, increases the risks for rhabdomyolysis to almost 6.0 per 10,000 person-years.[16] Most physicians have now abandoned routine monitoring of liver enzymes and creatine kinase, although they still consider this prudent in those on high-dose statins or in those on statin/fibrate combinations, and mandatory in the case of muscle cramps or of deterioration in renal function.
Consumption of grapefruit or grapefruit juice inhibits the metabolism of statins—furanocoumarins in grapefruit juice inhibit the cytochrome P450 enzyme CYP3A4, which is involved in the metabolism of most statins (however it is a major inhibitor of only lovastatin, simvastatin and to a lesser degree atorvastatin) and some other medications[21] (it had been thought that flavonoids were responsible). This increases the levels of the statin, increasing the risk of dose-related adverse effects (including myopathy/rhabdomyolysis). Consequently, consumption of grapefruit juice is not recommended in patients undergoing therapy with most statins. An alternative, somewhat risky, approach is that some users take grapefruit juice to enhance the effect of lower (hence cheaper) doses of statins. This is not recommended as a result of the increased risk and potential for statin toxicity.
[edit] Pharmacogenomics
A 2004 study showed that patients with one of two common single nucleotide polymorphisms (small genetic variations) in the HMG-CoA reductase gene were less responsive to statins.[22]
[edit] Mode of action
[edit] Cholesterol lowering
Most circulating cholesterol is manufactured internally, in amounts of about 1000 mg/day, via steroid biosynthesis through the HMG-CoA reductase pathway. Cholesterol, both from dietary intake and secreted into the duodenum as bile from the liver, is typically absorbed at a rate of 50% by the small intestines. The typical diet in the United States and many other Western countries is estimated as adding about 200–300 mg/day to intestinal intake, an amount much smaller than that secreted into the intestine in the bile. Thus internal production is an important factor.
Cholesterol is not water-soluble, and is therefore carried in the blood in the form of lipoproteins, the type being determined by the apoprotein, a protein coating that acts as an emulsifier. The relative balance between these lipoproteins is determined by various factors, including genetics, diet, and insulin resistance. Low density lipoprotein (LDL) and very low density lipoprotein (VLDL) carry cholesterol toward tissues, and elevated levels of these lipoproteins are associated with atheroma formation (fat-containing deposits in the arterial wall) and cardiovascular disease. Conversely, high density lipoprotein (HDL), carries cholesterol back to the liver and is associated with protection against cardiovascular disease.
Statins act by competitively inhibiting HMG-CoA reductase, the first committed enzyme of the HMG-CoA reductase pathway. By reducing intracellular cholesterol levels, they cause liver cells to make more LDL receptors, leading to increased clearance of low-density lipoprotein from the bloodstream.[23]
Direct evidence of the action of statin-based cholesterol lowering on atherosclerosis was presented in the ASTEROID trial, which demonstrated regression of atheroma employing intravascular ultrasound.[4]
[edit] Non-cholesterol related actions
Statins exhibit action beyond lipid-lowering activity in the prevention of atherosclerosis. Researchers hypothesize that statins prevent cardiovascular disease via four proposed mechanisms (all subjects of a large body of biomedical research):[24]
- Improve endothelial function
- Modulate inflammatory responses
- Maintain plaque stability
- Prevent thrombus formation
In 2008 the Jupiter study was halted early due to a large benefit seen in the statin treated group. This randomized placebo-controlled international study involved about 18,000 individuals with normal cholesterol and no history of heart disease, but with elevated C-reactive protein levels. Investigators found reductions in stroke, heart attack, and need for bypass surgery of about 50% in the statin treated group. There was also a 20% reduction in mortality. [25]
[edit] Controversy
Some scientists take a skeptical view of the need for many people to require statin treatment. Given the wide indications for which statins are prescribed, and the declining benefit in groups at lower baseline risk of cardiovascular events, the evidence base for expanded statin use has been questioned by some researchers.[26] A much smaller minority, exemplified by The International Network of Cholesterol Skeptics, question the "lipid hypothesis" itself and argue that elevated cholesterol has not been adequately linked to heart disease. These groups claim that statins are not as beneficial or safe as suggested.[27]
[edit] References
- ^ Endo A (11/01/1992). "The discovery and development of HMG-CoA reductase inhibitors" (PDF). J. Lipid Res. 33 (11): 1569–82. PMID 1464741. http://www.jlr.org/cgi/reprint/33/11/1569.
- ^ Law MR, Wald NJ, Rudnicka AR (June 2003). "Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis". BMJ 326 (7404): 1423. doi:. PMID 12829554. PMC: 162260. http://www.bmj.com/cgi/content/full/326/7404/1423.
- ^ Wilson P, D'Agostino R, Levy D, Belanger A, Silbershatz H, Kannel W (19 May 1998). "Prediction of coronary heart disease using risk factor categories". Circulation 97 (18): 1837–47. PMID 9603539. http://circ.ahajournals.org/cgi/content/full/97/18/1837.
- ^ a b Nissen S, Nicholls S, Sipahi I, Libby P, Raichlen J, Ballantyne C, Davignon J, Erbel R, Fruchart J, Tardif J, Schoenhagen P, Crowe T, Cain V, Wolski K, Goormastic M, Tuzcu E (2006). "Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial". JAMA 295 (13): 1556–65. doi:. PMID 16533939. http://jama.ama-assn.org/cgi/content/full/295/13/1556.
- ^ Wolozin, B; Wang SW, Li NC, Lee A, Lee TA, Kazis LE (July 19, 2007). "Simvastatin is associated with a reduced incidence of dementia and Parkinson's disease". BMC Medicine 5: 20. doi:. PMID 17640385. http://www.biomedcentral.com/1741-7015/5/20. Full text at PMC: 1955446
- ^ Khurana, V; Bejjanki HR, Caldito G, Owens MW (May 2007). "Statins reduce the risk of lung cancer in humans: a large case-control study of US veterans". Chest 131 (5): 1282–1288. doi:. PMID 17494779. http://www.chestjournal.org/cgi/content/full/131/5/1282.
- ^ Klein BE, Klein R, Lee KE, Grady LM (June 2006). "Statin use and incident nuclear cataract". JAMA 295 (23): 2752–8. doi:. PMID 16788130. http://jama.ama-assn.org/cgi/content/full/295/23/2752.
- ^ Golomb BA, Dimsdale JE, White HL, Ritchie JB, Criqui MH (April 2008). "Reduction in blood pressure with statins: results from the UCSD Statin Study, a randomized trial". Arch. Intern. Med. 168 (7): 721–7. doi:. PMID 18413554.
- ^ Shepherd J, Hunninghake DB, Barter P, McKenney JM, Hutchinson HG (2003). "Guidelines for lowering lipids to reduce coronary artery disease risk: a comparison of rosuvastatin with atorvastatin, pravastatin, and simvastatin for achieving lipid-lowering goals". Am. J. Cardiol. 91 (5A): 11C–17C; discussion 17C–19C. doi:. PMID 12646338.
- ^ Zhou Z, Rahme E, Pilote L (2006). "Are statins created equal? Evidence from randomized trials of pravastatin, simvastatin, and atorvastatin for cardiovascular disease prevention". Am. Heart J. 151 (2): 273–81. doi:. PMID 16442888.
- ^ Jones P, Kafonek S, Laurora I, Hunninghake D (1998). "Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study)". Am J Cardiol 81 (5): 582–7. doi:. PMID 9514454.
- ^ Consumer Reports Health.org, Statins: Summary of Recommendations. February 2007
- ^ Ghirlanda G, Oradei A, Manto A, Lippa S, Uccioli L, Caputo S, Greco A, Littarru G (1993). "Evidence of plasma CoQ10-lowering effect by HMG-CoA reductase inhibitors: a double-blind, placebo-controlled study". J Clin Pharmacol 33 (3): 226–9. PMID 8463436.
- ^ Marcoff L, Thompson PD (2007). "The role of coenzyme Q10 in statin-associated myopathy: a systematic review". J. Am. Coll. Cardiol. 49 (23): 2231–7. doi:. PMID 17560286.
- ^ "SLCO1B1 Variants and Statin-Induced Myopathy -- A Genomewide Study". N. Engl. J. Med. Online: 789. July 2008. doi:. PMID 18650507. http://content.nejm.org/cgi/content/full/NEJMoa0801936v1.
- ^ a b Graham DJ, Staffa JA, Shatin D, et al (2004). "Incidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs". JAMA 292 (21): 2585–90. doi:. PMID 15572716. http://jama.ama-assn.org/cgi/content/full/292/21/2585.
- ^ Hanai J, Cao P, Tanksale P, et al (2007). "The muscle-specific ubiquitin ligase atrogin-1/MAFbx mediates statin-induced muscle toxicity". J. Clin. Invest. 117 (12): 3940–51. doi:. PMID 17992259.
- ^ Dale KM, Coleman CI, Henyan NN, Kluger J, White CM (2006). "Statins and cancer risk: a meta-analysis". JAMA 295 (1): 74–80. doi:. PMID 16391219. http://jama.ama-assn.org/cgi/content/full/295/1/74.
- ^ Poynter JN, Gruber SB, Higgins PD, et al (2005). "Statins and the risk of colorectal cancer". N. Engl. J. Med. 352 (21): 2184–92. doi:. PMID 15917383. http://content.nejm.org/cgi/content/full/352/21/2184.
- ^ Alsheikh-Ali AA (2007). "Effect of the Magnitude of Lipid Lowering on Risk of Elevated Liver Enzymes, Rhabdomyolysis, and Cancer: Insights From Large Randomized Statin Trials". Journal of the American College of Cardiology 50 (5): 409–418. doi:. PMID 17662392.
- ^ Kane GC, Lipsky JJ (2000). "Drug-grapefruit juice interactions". Mayo Clin. Proc. 75 (9): 933–42. doi:. PMID 10994829.
- ^ Chasman DI, Posada D, Subrahmanyan L, Cook NR, Stanton VP, Ridker PM (2004). "Pharmacogenetic study of statin therapy and cholesterol reduction". JAMA 291 (23): 2821–7. doi:. PMID 15199031. http://jama.ama-assn.org/cgi/content/full/291/23/2821.
- ^ Ma PT, Gil G, Südhof TC, Bilheimer DW, Goldstein JL, Brown MS (1986). "Mevinolin, an inhibitor of cholesterol synthesis, induces mRNA for low density lipoprotein receptor in livers of hamsters and rabbits" (PDF). Proc. Natl. Acad. Sci. U.S.A. 83 (21): 8370–4. doi:. PMID 3464957. http://www.pnas.org/cgi/reprint/83/21/8370. Full text at PMC: 386930
- ^ Furberg CD (19 Jan 1999). "Natural Statins and Stroke Risk". Circulation 99 (2): 185–188. PMID 9892578. http://circ.ahajournals.org/cgi/content/full/99/2/185.
- ^ Ridler PM, Danielson E, Fonseca FAH, et al. (2008). "Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein". NEJM 359: 2195–207. doi:. PMID 18997196. http://content.nejm.org/cgi/reprint/NEJMoa0807646v1.pdf.
- ^ Abramson J, Wright J (2007). "Are lipid-lowering guidelines evidence-based?". Lancet 369 (9557): 168–9. doi:. PMID 17240267.
- ^ Ravnskov U, Rosch P, Sutter M, Houston M (2006). "Should we lower cholesterol as much as possible?". BMJ 332 (7553): 1330–2. doi:. PMID 16740566. http://www.bmj.com/cgi/content/full/332/7553/1330.
[edit] External links
- Statin page at Bandolier, an evidence-based medicine journal
|
||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||