Penicillin
From Wikipedia, the free encyclopedia
Penicillin (sometimes abbreviated PCN or pen) is a group of antibiotics derived from Penicillium fungi.[1] They are Beta-lactam antibiotics used in the treatment of bacterial infections caused by susceptible, usually Gram-positive, organisms.
The term "penicillin" can also refer to the mixture of substances that are naturally produced.[2]
The term Penam is used to describe the core skeleton of a member of a penicillin antibiotic. This skeleton has the molecular formula R-C9H11N2O4S, where R is a variable side chain.
Contents |
[edit] History
[edit] Discovery
The discovery of penicillin is attributed to Scottish scientist and nobel laureate Alexander Fleming in 1928. He showed that if Penicillium notatum was grown in the appropriate substrate, it would exude a substance with antibiotic properties, which he dubbed "penicillin". This serendipitous observation began the modern era of antibiotic discovery. The development of penicillin for use as a medicine is attributed to the Australian Nobel Laureate Howard Walter Florey.
However, several others reported the bacteriostatic effects of Penicillium earlier than Fleming. The first published reference appears in the publication of the Royal Society in 1875, by John Tyndall.[3] Ernest Duchesne documented it in an 1897 paper, which was not accepted by the Institut Pasteur because of his youth. In March 2000, doctors at the San Juan de Dios Hospital in San José, Costa Rica published the manuscripts of the Costa Rican scientist and medical doctor Clodomiro (Clorito) Picado Twight (1887–1944). They reported Picado's observations on the inhibitory actions of fungi of the genus Penic between 1915 and 1927. Picado reported his discovery to the Paris Academy of Sciences, yet did not patent it, even though his investigations started years before Fleming's.
Fleming recounted that the date of his breakthrough was on the morning of Friday, September 28, 1928.[4] It was an example of fortuitous accident: In his laboratory in the basement of St. Mary's Hospital in London (now part of Imperial College), Fleming noticed a petri dish containing Staphylococcus plate culture he'd mistakenly left open, which was contaminated by blue-green mould. There was a halo of inhibited bacterial growth around it. Fleming concluded that the mould was releasing a substance that was repressing the growth and lysing the bacteria. He grew a pure culture and discovered that it was a Penicillium mould, now known to be Penicillium notatum. Charles Thom, an American specialist working at the U.S. Department of Agriculture, was the acknowledged expert, and Fleming referred the matter to him. Fleming coined the term "penicillin" to describe the filtrate of a broth culture of the Penicillium mould. Even in these early stages, penicillin was found to be most effective against Gram-positive bacteria, and ineffective against Gram-negative organisms and fungi. He expressed initial optimism that penicillin would be a useful disinfectant, being highly potent with minimal toxicity compared to antiseptics of the day, and noted its laboratory value in the isolation of "Bacillus influenzae" (now Haemophilus influenzae).[5] After further experiments, Fleming was convinced that penicillin could not last long enough in the human body to kill pathogenic bacteria, and stopped studying it after 1931. He restarted clinical trials in 1934, and continued to try to get someone to purify it until 1940.[6]
[edit] Medical Application
In 1930 Cecil George Paine, a pathologist at the Royal Infirmary in Sheffield, attempted to use penicillin to treat sycosis barbae–eruptions in beard follicles–but was unsuccessful, probably because the drug did not penetrate the skin deeply enough. Moving on to ophthalmia neonatorum–a gonococcal infection in infants–he achieved the first recorded cure with penicillin, on 25 November 1930. He then cured four additional patients (one adult and three infants) of eye infections, failing to cure a fifth.[7]
In 1939, Australian scientist Howard Florey (later Baron Florey) and a team of researchers (Ernst Boris Chain, A. D. Gardner, Norman Heatley, M. Jennings, J. Orr-Ewing and G. Sanders) at the Sir William Dunn School of Pathology, University of Oxford made significant progress in showing the in vivo bactericidal action of penicillin. Their attempts to treat humans failed due to insufficient volumes of penicillin (the first patient treated was Reserve Constable Albert Alexander), but they proved it harmless and effective on mice.[8]
Some of the pioneering trials of penicillin took place at the Radcliffe Infirmary in Oxford, England. On March 14, 1942, John Bumstead and Orvan Hess successfully treated a patient using penicillin.[9][10] These trials continue to be cited by some sources as the first cures using penicillin, though the Paine trials took place earlier.[11]
[edit] Mass Production
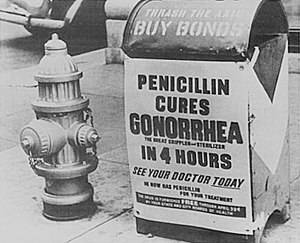
The challenge of mass-producing the drug was daunting. On March 14, 1942 the first patient was treated for streptococcal septicemia with U.S.-made penicillin produced by Merck & Co.[12] Half of the total supply produced at the time was used on that one patient. By June 1942 there was just enough U.S. penicillin available to treat ten patients.[13] A moldy cantaloupe in a Peoria, Illinois market in 1943 was found to contain the best and highest-quality penicillin after a worldwide search.[14] The discovery of the cantaloupe, and the results of fermentation research on corn-steep liquid at the Northern Regional Research Laboratory at Peoria, Illinois, allowed the USA to produce 2.3 million doses in time for the invasion of Normandy in the spring of 1944. Large-scale production resulted from the development of deep-tank fermentation by chemical engineer Margaret Hutchinson Rousseau.[15]
During World War II, penicillin made a major difference in the number of deaths and amputations caused by infected wounds among Allied forces, saving an estimated 12%–15% of lives.[citation needed] Availability was severely limited, however, by the difficulty of manufacturing large quantities of penicillin and by the rapid renal clearance of the drug, necessitating frequent dosing. Penicillin is actively secreted, and about 80% of a penicillin dose is cleared from the body within three to four hours of administration. Indeed, during the early penicillin era, the drug was so scarce and so highly valued that it became common to collect the urine from patients being treated, so that the penicillin in the urine could be isolated and reused.[16]
This was not a satisfactory solution, so researchers looked for a way to slow penicillin secretion. They hoped to find a molecule that could compete with penicillin for the organic acid transporter responsible for secretion, such that the transporter would preferentially secrete the competing molecule and the penicillin would be retained. The uricosuric agent probenecid proved to be suitable. When probenecid and penicillin are administered together, probenecid competitively inhibits the secretion of penicillin, increasing penicillin's concentration and prolonging its activity. Eventually, the advent of mass-production techniques and semi-synthetic penicillins resolved the supply issues, so this use of probenecid declined.[16] Probenecid is still useful, however, for certain infections requiring particularly high concentrations of penicillins.[17]
[edit] Chemical Structure
The chemical structure of penicillin was determined by Dorothy Crowfoot Hodgkin in the early 1940s. A team of Oxford research scientists led by Australian Howard Florey, Baron Florey and including Ernst Boris Chain and Norman Heatley discovered a method of mass-producing the drug. Chemist Robert Burns Woodward at Harvard University completed the first total synthesis of penicillin and some of its analogs in the early 1950s, but his methods were not efficient for mass production. Florey and Chain shared the 1945 Nobel prize in medicine with Fleming for their work, and, after WWII, Australia was the first country to make the drug available for civilian use. Penicillin has since become the most widely used antibiotic to date, and is still used for many Gram-positive bacterial infections.
[edit] Developments from penicillin
The narrow range of treatable diseases or spectrum of activity of the penicillins, along with the poor activity of the orally active phenoxymethylpenicillin, led to the search for derivatives of penicillin that could treat a wider range of infections.
The first major development was ampicillin, which offered a broader spectrum of activity than either of the original penicillins. Further development yielded beta-lactamase-resistant penicillins including flucloxacillin, dicloxacillin and methicillin. These were significant for their activity against beta-lactamase-producing bacteria species, but are ineffective against the methicillin-resistant Staphylococcus aureus strains that subsequently emerged.
Another development of the line of true penicillins was the antipseudomonal penicillins, such as ticarcillin and piperacillin, useful for their activity against Gram-negative bacteria. However, the usefulness of the beta-lactam ring was such that related antibiotics, including the mecillinams, the carbapenems and, most important, the cephalosporins, still retain it at the center of their structures.[18]
[edit] Mechanism of action
β-lactam antibiotics work by inhibiting the formation of peptidoglycan cross-links in the bacterial cell wall. The β-lactam moiety (functional group) of penicillin binds to the enzyme (DD-transpeptidase) that links the peptidoglycan molecules in bacteria, which weakens the cell wall of the bacterium (in other words, the antibiotic causes cytolysis or death due to osmotic pressure). In addition, the build-up of peptidoglycan precursors triggers the activation of bacterial cell wall hydrolases and autolysins, which further digest the bacteria's existing peptidoglycan.
Gram-positive bacteria are called protoplasts when they lose their cell wall. Gram-negative bacteria do not lose their cell wall completely and are called spheroplasts after treatment with penicillin.
Penicillin shows a synergistic effect with aminoglycosides, since the inhibition of peptidoglycan synthesis allows aminoglycosides to penetrate the bacterial cell wall more easily, allowing its disruption of bacterial protein synthesis within the cell. This results in a lowered MBC for susceptible organisms.
Penicillins, like other β-lactam antibiotics, not only block the division of bacteria, including cyanobacteria, but also the division of cyanelles, the photosynthetic organelles of the Glaucophytes, and the division of chloroplasts of bryophytes. In contrast, they have no effect on the plastids of the highly developed vascular plants. This is supporting the endosymbiotic theory and indicates an evolution of plastid division in land plants.[19]
[edit] Variants in clinical use
The term “penicillin” is often used in the generic sense to refer to one of the narrow-spectrum penicillins, in particular, benzylpenicillin (penicillin G).
Other types include:
[edit] Adverse effects
Common adverse drug reactions (≥1% of patients) associated with use of the penicillins include diarrhea, hypersensitivity, nausea, rash, neurotoxicity urticaria, and/or superinfection (including candidiasis). Infrequent adverse effects (0.1–1% of patients) include fever, vomiting, erythema, dermatitis, angioedema, seizures (especially in epileptics), and/or pseudomembranous colitis.[17]
Pain and inflammation at the injection site is also common for parenterally administered benzathine benzylpenicillin, benzylpenicillin, and, to a lesser extent, procaine benzylpenicillin.
Although penicillin is still the most commonly reported allergy, less than 20% of all patients who believe that they have a penicillin allergy are truly allergic to penicillin;[20] nevertheless, penicillin is still the most common cause of severe allergic drug reactions.
Allergic reactions to any β-lactam antibiotic may occur in up to 10% of patients receiving that agent.[21] Anaphylaxis will occur in approximately 0.01% of patients.[17] It has previously been accepted that there was up to a 10% cross-sensitivity between penicillin-derivatives, cephalosporins, and carbapenems, due to the sharing of the β-lactam ring.[22][23] However recent assessments have shown no increased risk for cross-allergy for 2nd generation or later cephalosporins.[24][25] Recent papers have shown that a major feature in determining immunological reactions is the similarity of the side chain of first generation cephalosporins to penicillins, rather than the β-lactam structure that they share.[26]
[edit] Production
Penicillin is a secondary metabolite of fungus Penicillium, that is produced when growth of the fungus is inhibited by stress. It is not produced during active growth. Production is also limited by feedback in the synthesis pathway of penicillin.
-
- α-ketoglutarate + AcCoA → homocitrate → L-α-aminoadipic acid → L-Lysine + β-lactam
The by-product L-Lysine inhibits the production of homocitrate, so the presence of exogenous lysine should be avoided in penicillin production.
The penicillium cells are grown using a technique called fed-batch culture, in which the cells are constantly subject to stress and will produce plenty of penicillin. The carbon sources that are available are also important: glucose inhibits penicillin, whereas lactose does not. The pH level, nitrogen level, Lysine level, Phosphate level, and oxygen availability of the batches must be controlled automatically.
Penicillin production emerged as an industry as a direct result of World War II. During the war, there was an abundance of jobs available on the home front. A War Production Board was founded to monitor job distribution and production.[27] Penicillin was produced in huge quantities during the war and the industry prospered. In July 1943, the War Production Board drew up a plan for the mass distribution of penicillin stocks to troops fighting in Europe. At the time of this plan, 425 million units per year were being produced. As a direct result of the war and the War Production Board, by June 1945 over 646 billion units per year were being produced.[28]
In recent years, the biotechnology method of directed evolution has been applied to produce by mutation a large number of penicillin strains. These directed-evolution techniques include error-prone PCR, DNA shuffling, ITCHY, and strand overlap PCR.
[edit] See also
[edit] References
- ^ penicillin at Dorland's Medical Dictionary
- ^ "penicillin - Definition from Merriam-Webster's Medical Dictionary". http://medical.merriam-webster.com/medical/penicillin. Retrieved on 2009-01-02.
- ^ Phil. Trans., 1876, 166, pp27-74. Referred to at: Discoveries of anti-bacterial effects of penicillium moulds before Fleming
- ^ Haven, Kendall F. (1994). Marvels of Science : 50 Fascinating 5-Minute Reads. Littleton, Colo: Libraries Unlimited. pp. 182. ISBN 1-56308-159-8.
- ^ Fleming A. (1929). "On the antibacterial action of cultures of a penicillium, with special reference to their use in the isolation of B. influenzæ". Br J Exp Pathol 10 (31): 226–36.
- ^ Brown, Kevin. (2004). Penicillin Man: Alexander Fleming and the Antibiotic Revolution.. Stroud: Sutton. ISBN 0-7509-3152-3.
- ^ Wainwright, M & Swan, HT (1986 January). "C.G. Paine And The Earliest Surviving Clinical Records Of Penicillin Therapy". Medical History 30 (1): 42–56. PMID 3511336.
- ^ Drews, Jürgen (March 2000). "Drug Discovery: A Historical Perspective". Science 287 (5460): 1960–4. doi:. PMID 10720314.
- ^ Saxon, W. (June 9, 1999). "Anne Miller, 90, first patient who was saved by penicillin". The New York Times. http://query.nytimes.com/gst/fullpage.html?res=9E0DE7D91139F93AA35755C0A96F958260.
- ^ Krauss K, editor (1999). "Yale-New Haven Hospital Annual Report". written at New Haven (PDF). Yale-New Haven Hospital. http://www.ynhh.org/general/annreport/ynhh99ar.pdf.
- ^ Wainwright, M & Swan, HT (1986 January). "C.G. Paine And The Earliest Surviving Clinical Records Of Penicillin Therapy". Medical History 30 (1): 42–56. PMID 3511336.
- ^ The First Use of Penicillin in the United States, by Charles M. Grossman. Annals of Internal Medicine 15 July 2008: Volume 149, Issue 2, Pages 135-136.
- ^ John S. Mailer, Jr., and Barbara Mason. "Penicillin : Medicine's Wartime Wonder Drug and Its Production at Peoria, Illinois". lib.niu.edu. http://www.lib.niu.edu/ipo/2001/iht810139.html. Retrieved on 2008-02-11.
- ^ Mary Bellis. "The History of Penicillin". Inventors. About.com. http://inventors.about.com/od/pstartinventions/a/Penicillin.htm. Retrieved on 2007-10-30.
- ^ Chemical Heritage Manufacturing a Cure: Mass Producing Penicillin
- ^ a b Silverthorn, DU. (2004). Human physiology: an integrated approach. (3rd ed.). Upper Saddle River (NJ): Pearson Education. ISBN 0-8053-5957-5.
- ^ a b c Rossi S, editor, ed (2006). Australian Medicines Handbook. Adelaide: Australian Medicines Handbook. ISBN 0-9757919-2-3.
- ^ James, PharmD, Christopher W.; Cheryle Gurk-Turner, RPh (2001 January). "Cross-reactivity of beta-lactam antibiotics". Baylor University Medical Center Proceedings (Dallas, Texas: Baylor University Medical Center) 14 (1): 106–7. PMID 16369597.
- ^ Kasten, Britta; Reski, Ralf (30 Mar 1997). "β-lactam antibiotics inhibit chloroplast division in a moss (Physcomitrella patens) but not in tomato (Lycopersicon esculentum)". Journal of Plant Physiology 150 (1-2): 137–140. http://cat.inist.fr/?aModele=afficheN&cpsidt=2640663.
- ^ Salkind AR, Cuddy PG, Foxworth JW (2001). "Is this patient allergic to penicillin? An evidence-based analysis of the likelihood of penicillin allergy". JAMA 285 (19): 2498–505. doi:. PMID 11368703.
- ^ Solensky R (2003). "Hypersensitivity reactions to beta-lactam antibiotics". Clinical reviews in allergy & immunology 24 (3): 201–20. doi:. PMID 12721392.
- ^ Dash CH (1975). "Penicillin allergy and the cephalosporins". J. Antimicrob. Chemother. 1 (3 Suppl): 107–18. PMID 1201975.
- ^ Gruchalla RS, Pirmohamed M (2006). "Clinical practice. Antibiotic allergy". N. Engl. J. Med. 354 (6): 601–9. doi:. PMID 16467547.
- ^ Pichichero ME (2006). "Cephalosporins can be prescribed safely for penicillin-allergic patients" (PDF). The Journal of family practice 55 (2): 106–12. PMID 16451776. http://www.jfponline.com/pdf%2F5502%2F5502JFP_AppliedEvidence1.pdf.
- ^ Pichichero ME (2007). "Use of selected cephalosporins in penicillin-allergic patients: a paradigm shift". Diagn. Microbiol. Infect. Dis. 57 (3 Suppl): 13S–8S. doi:. PMID 17349459.
- ^ Antunez C, Blanca-Lopez N, Torres MJ, et al (2006). "Immediate allergic reactions to cephalosporins: evaluation of cross-reactivity with a panel of penicillins and cephalosporins". J Allergy Clin. Immunol. 117 (2): 404–10. doi:. PMID 16461141.
- ^ "Start of World War II." Legacy Publishers. 2 Apr. 2008
- ^ Parascandola, John (1980). The History of antibiotics: a symposium. American Institute of the History of Pharmacy No. 5. ISBN 0-931292-08-5.
[edit] External links