Dextromethorphan
From Wikipedia, the free encyclopedia
 |
|
 |
|
|
Dextromethorphan
|
|
| Systematic (IUPAC) name | |
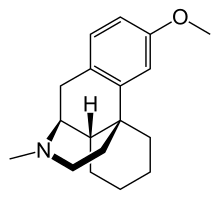
| ((+)-3-methoxy-17-methyl- (9α,13α,14α)-morphinan) | |
| Identifiers | |
| CAS number | |
| ATC code | R05 |
| PubChem | |
| DrugBank | |
| ChemSpider | |
| Chemical data | |
| Formula | C18H25NO |
| Mol. mass | 271.4 g/mol |
| SMILES | & |
| Physical data | |
| Melt. point | 111 °C (232 °F) |
| Pharmacokinetic data | |
| Bioavailability | 11%[1] |
| Metabolism | Hepatic (liver) enzymes: major CYP2D6, minor CYP3A4, and minor CYP3A5 |
| Half life | 1.4–3.9 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status | |
| Routes | Oral |
Dextromethorphan (DXM or DM) is an antitussive drug. It is one of the active ingredients used to prevent coughs in many over-the-counter cold and cough medicines. Dextromethorphan has also found other uses in medicine, ranging from pain relief to psychological applications. It is sold in syrup, tablet, and lozenge forms manufactured under several different brand names and generic labels. In its pure form, dextromethorphan occurs as a white powder.
When exceeding label-specified maximum dosages, dextromethorphan acts as a dissociative hallucinogenic drug. Its mechanism of action is as an NMDA receptor antagonist, producing effects similar to those of the controlled substances ketamine and phencyclidine (PCP). [2]
Contents |
[edit] History
Dextromethorphan was first patented under U.S. Patent 2,676,177. The FDA approved dextromethorphan for over-the-counter sale as a cough suppressant in 1958. This filled the need for a cough suppressant lacking the sedative side-effects, stronger potential for abuse, and physically addictive properties of codeine phosphate, the most widely-used cough medication at the time.[3] Codeine phosphate syrup is still available in small doses without a prescription in some states, but requires a signature and ID to purchase, similar to pseudoephedrine. As with most cough suppressants, studies show that dextromethorphan's effectiveness is highly debatable,[4] especially in children.[5]
During the 1960s and 1970s, dextromethorphan became available in an over-the-counter tablet form by the brand name Romilar. In 1973, Romilar was taken off the shelves after a burst in sales due to frequent abuse, and was replaced by cough syrup in an attempt to cut down on abuse.[3]
More recently (the early 1990s) gel capsule forms began reappearing in the form of Drixoral Cough Liquid Caps and later Robitussin CoughGels as well as several generic forms of that preparation.
[edit] Chemistry
Dextromethorphan is the dextrorotatory enantiomer of the methyl ether of levorphanol, a narcotic analgesic. It is also a stereoisomer of levomethorphan, an opioid analgesic. It is named according to IUPAC rules as (+)-3-methoxy-17-methyl-9α,13α,14α-morphinan. As the pure free base, dextromethorphan occurs as an odorless, white to slightly yellow crystalline powder. It is freely soluble in chloroform and essentially insoluble in water. Commercially, dextromethorphan is commonly available as the monohydrated hydrobromide salt, although some newer extended-release formulations contain dextromethorphan bound to an ion exchange resin based on polystyrene sulfonic acid. Dextromethorphan's specific rotation in water is +27.6° (20°C, Sodium D-line).
[edit] Indications
The primary use of dextromethorphan is as a cough suppressant, for the temporary relief of cough caused by minor throat and bronchial irritation (as commonly accompanies the common cold), as well as other causes such as inhaled irritants.
Additionally, a combination of dextromethorphan and quinidine has been shown to alleviate symptoms of easy laughing and crying (pseudobulbar affect) in patients with amyotrophic lateral sclerosis and multiple sclerosis.[6] Dextromethorphan is also being investigated as a possible treatment for neuropathic pain and pain associated with fibromyalgia.[7]
[edit] Pharmacokinetics
At therapeutic doses, dextromethorphan acts centrally (meaning that it acts on the brain) as opposed to locally (on the respiratory tract). It elevates the threshold for coughing, without inhibiting ciliary activity. Dextromethorphan is rapidly absorbed from the gastrointestinal tract and converted into an active metabolite, dextrorphan, within 15 to 60 minutes of ingestion[citation needed]. The average dosage necessary for effective antitussive therapy is between 10 mg and 45 mg, depending on the individual. The duration of action after oral administration is approximately three to eight hours for dextromethorphan-hydrobromide, and ten to twelve hours for dextromethorphan-polistirex.
Because administration of dextromethorphan can trigger a histamine release (an allergic reaction), its use in atopic children is very limited.
[edit] Side-effects
Side-effects of dextromethorphan use can include:[8]
|
|
Dextromethorphan can also cause other gastrointestinal disturbances. When injected directly into the blood stream, some studies suggest that dextromethorphan has the potential to cause Olney's Lesions.[9][10] In some rare documented cases, dextromethorphan has produced psychological dependence in people who abused it. However, it does not produce physical addiction, according to the WHO Committee on Drug Dependence.[11]
[edit] Drug interactions
Dextromethorphan should not be taken with either of the following:
CNS depressant drugs and substances, including alcohol, antihistamines, and some psychotropics, will have a cumulative CNS depressant effect if taken with dextromethorphan.[8]
[edit] Contraindications
Because dextromethorphan can trigger a histamine release (allergic reaction), atopic children, who are especially susceptible to allergic reactions, should be administered dextromethorphan only if absolutely necessary, and only under the strict supervision of a health care professional.[8]
[edit] Clinical pharmacology
Following oral administration, dextromethorphan is rapidly absorbed from the gastrointestinal tract, where it enters the bloodstream and crosses the blood-brain barrier.
[edit] Nervous system activity
- NMDA receptor antagonist
- σ1 and σ2 sigma receptor agonist.[12]
- α3β4 nicotinic receptor antagonist[13]
- Serotonin releaser (NOT reuptake inhibitor), likely through NMDA antagonism[14] [15]
- Dopamine reuptake inhibitor (disputed)[8][16]
- NADPH oxidase inhibitor [17]
[edit] Metabolism
The first-pass through the hepatic portal vein results in some of the drug being metabolized by O-demethylation into an active metabolite of dextromethorphan called dextrorphan (DXO). DXO is the 3-hydroxy derivative of dextromethorphan. The therapeutic activity of dextromethorphan is believed to be caused by both the drug and this metabolite. Dextromethorphan also undergoes N-demethylation (to 3-methoxymorphinan or MEM),[18] and partial conjugation with glucuronic acid and sulfate ions. Hours after dextromethorphan therapy, (in humans) the metabolites (+)-3-hydroxy-N-methylmorphinan, (+)-3-morphinan, and traces of the unchanged drug are detectable in the urine.[8]
A major metabolic catalyst involved is the cytochrome P450 enzyme known as 2D6, or CYP2D6. A significant portion of the population has a functional deficiency in this enzyme and are known as poor CYP2D6 metabolizers. O-demethylation of DXM to DXO contributes to at least 80% of the DXO formed during DXM metabolism.[18] As CYP2D6 is a major metabolic pathway in the inactivation of dextromethorphan, the duration of action and effects of dextromethorphan can be increased by as much as three times in such poor metabolizers.[19] In one study on 252 Americans, 84.3% were found to be "fast" (extensive) metabolizers, 6.8% to be "intermediate" metabolizers, and 8.8% were "slow" metabolizers of DXM. [20] There are a number of known alleles for CYP2D6, including several completely inactive variants. The distribution of alleles is uneven amongst ethnic groups; see also CYP2D6 - Ethnic factors in variability.
A large number of medications are potent inhibitors of CYP2D6. Some types of medications known to inhibit CYP2D6 include certain SSRI and tricyclic antidepressants, some antipsychotics, and the commonly available antihistamine diphenhydramine -- also known as Benadryl. There exists, therefore, the potential of interactions between dextromethorphan and medications which inhibit this enzyme, particularly in slow metabolizers. See also CYP2D6 - Ligands.
DXM is also metabolized by CYP3A4. N-demethylation is primarily accomplished by CYP3A4, contributing to at least 90% of the MEM formed as a primary metabolite of DXM.[18]
A number of other CYP enzymes are implicated as minor pathways of DXM metabolism. CYP2B6 is actually more effective than CYP3A4 at N-demethylation of DXM, but since the average individual has a much lower CYP2B6 content in their liver relative to CYP3A4, most N-demethylation of DXM is catalyzed by CYP3A4.[18]
[edit] Recreational use
Since their introduction, over-the-counter preparations containing dextromethorphan have been used in a manner inconsistent with their labeling, often as a recreational drug.[3] At doses higher than medically recommended, dextromethorphan is classified as a dissociative hallucinogenic drug, with visible effects that are similar to ketamine and phencyclidine (PCP). It can produce distortions of the visual field, feelings of dissociation, perceived bodily distortion, and excitement. [21] [22]
[edit] References
- ^ "Plasma profile and pharmacokinetics of dextromethorphan after intravenous and oral administration". Journal of Veterinary Pharmacology and Therapeutics. http://www.blackwell-synergy.com/doi/abs/10.1111/j.1365-2885.2004.00608.x?cookieSet=1&journalCode=jvp.
- ^ DEXTROMETHORPHAN (Street Names: DXM, CCC, Triple C, Skittles, Robo, Poor Man’s PCP)
- ^ a b c Dextromethorphan (DXM) | CESAR
- ^ Cough medicines "have no benefit" BBC News: Health, Tuesday, July 6, 2004. Accessed July 28, 2007.
- ^ [1] "Kids' cough medicine no better than placebo" San Francisco Chronicle, July 8, 2004
- ^ Brooks B, Thisted R, Appel S, Bradley W, Olney R, Berg J, Pope L, Smith R (2004). "Treatment of pseudobulbar affect in ALS with dextromethorphan/quinidine: a randomized trial". Neurology 63 (8): 1364–70. PMID 15505150.
- ^ "Cough Drug May Help Fibromyalgia Pain". WebMD. http://www.webmd.com/content/article/106/108142.
- ^ a b c d e f g "Dextromethorphan". NHTSA. http://www.nhtsa.dot.gov/PEOPLE/injury/research/job185drugs/dextromethorphan.htm.
- ^ Olney J, Labruyere J, Price M (1989). "Pathological changes induced in cerebrocortical neurons by phencyclidine and related drugs". Science 244 (4910): 1360–2. doi:. PMID 2660263.
- ^ Hargreaves R, Hill R, Iversen L. "Neuroprotective NMDA antagonists: the controversy over their potential for adverse effects on cortical neuronal morphology". Acta Neurochir Suppl (Wien) 60: 15–9. PMID 7976530.
- ^ WHO Expert Committee on Drug Dependence (1970) ( PDF). Seventeenth Report. World Health Organization. http://whqlibdoc.who.int/trs/WHO_TRS_437.pdf. Retrieved on 2008-12-29.
- ^ "British Journal of Pharmacology — The dextromethorphan analog dimemorfan attenuates kainate-induced seizures via [sigma1 receptor activation: comparison with the effects of dextromethorphan"]. http://www.nature.com/bjp/journal/v144/n7/full/0705998a.html. Retrieved on 2007-07-16.
- ^ Hernandez SC, Bertolino M, Xiao Y, Pringle KE, Caruso FS, Kellar KJ (2000). "Dextromethorphan and its metabolite dextrorphan block alpha3beta4 neuronal nicotinic receptors". J. Pharmacol. Exp. Ther. 293 (3): 962–7. PMID 10869398.
- ^ Kamei J, Mori T, Igarashi H, Kasuya Y (1992). "Serotonin release in nucleus of the solitary tract and its modulation by antitussive drugs". Res. Commun. Chem. Pathol. Pharmacol. 76 (3): 371–4. PMID 1636059.
- ^ A Płaźnik, M Jessa, M Nazar (1997). The behavioral effects of NMDA antagonists in serotonin depleted rats. PMID 9264085.
- ^ Verma A, Moghaddam B (16 January 1996). "NMDA receptor antagonists impair prefrontal cortex function as assessed via spatial delayed alternation performance in rats: modulation by dopamine". Journal of Neuroscience 1: 373–9.
- ^ Zhang W, Wang T, Qin L, Gao HM, Wilson B, Ali SF, Zhang W, Hong JS, Liu B (20 January 2004). "Neuroprotective effect of dextromethorphan in the MPTP Parkinson's disease model: role of NADPH oxidase". The FASEB Journal. PMID 14734632.
- ^ a b c d "Comparative Contribution to Dextromethorphan Metabolism by Cytochrome P450 Isoforms in Vitro: Can Dextromethorphan Be Used as a Dual Probe for Both CYP2D6 and CYP3A Activities?". http://dmd.aspetjournals.org/cgi/content/full/29/11/1514. Retrieved on 2008-08-10.
- ^ "Clinical Pharmacology & Therapeutics — Abstract of article: The influence of CYP2D6 polymorphism and quinidine on the disposition and antitussive effect of dextromethorphan in humans[ast"]. http://www.nature.com/clpt/journal/v60/n3/abs/clpt1996482a.html. Retrieved on 2007-07-16.
- ^ "The polymorphic metabolism of dextromethorphan (abstract)". http://jcp.sagepub.com/cgi/content/abstract/27/2/139. Retrieved on 2008-08-10.
- ^ AJ Giannini. Drugs of Abuse--Second Edition. Los Angeles, Practice Management Information Corp, 1997.
- ^ [ http://dxmunderground.ning.com]
[edit] See also
| Wikimedia Commons has media related to: Dextromethorphan |
|
||||||||||||||||
|
|||||||||||

