Anthrax
From Wikipedia, the free encyclopedia
| This article may require copy-editing for grammar, style, cohesion, tone or spelling. You can assist by editing it now. A how-to guide is available. (March 2009) |
| Anthrax Classification and external resources |
|
| Microphotograph of a Gram stain the bacterium Bacillus anthracis which causes anthrax. | |
| ICD-10 | A22.minor |
| ICD-9 | 022 |
| OMIM | [2] 606410 608041 |
| DiseasesDB | 1203 |
| MedlinePlus | 001325 |
| eMedicine | med/148 |
| MeSH | D000881 |
Anthrax is an acute disease in humans and animals caused by Bacillus anthracis, which is highly lethal in all forms. There are effective vaccines against anthrax, and some forms of the disease respond well to antibiotic treatment.
The anthrax bacillus is one of only a few that can form long-lived spores: in a hostile environment, caused perhaps by the death of an infected host or extremes of temperature, the bacteria produce inactive dormant spores which can remain viable for many decades and perhaps centuries. These spores are found on all continents except Antarctica. When spores are inhaled, ingested, or come into contact with a skin lesion on a host they reactivate and multiply rapidly.
Anthrax most commonly infects wild and domesticated herbivorous mammals which ingest or inhale the spores while eating grass or browsing. Ingestion is assumed to be the most common route by which herbivores contract anthrax, but this is yet to be proven. Carnivores living in the same environment may ingest infected animals and become infected themselves. Anthrax can also infect humans when they are exposed to blood and other tissues from infected animals (via inhalation or direct inoculation through broken skin), eat tissue from infected animals, or are exposed to a high density of anthrax spores from an animal's fur, hide, or wool.
Anthrax spores can be grown in vitro and used as a biological weapon. Anthrax does not spread directly from one infected animal or person to another, but spores can be transported by clothing, shoes etc.; and the body of a mammal that died of anthrax can be a very dangerous source of anthrax spores.
The name anthrax comes from anthrakitis, the Greek word for anthracite (coal), in reference to the black skin lesions victims develop in a cutaneous skin infection.
Contents |
[edit] Overview

Anthrax is one of the oldest recorded diseases of grazing animals such as sheep and cattle and is believed to be the Sixth Plague mentioned in the Book of Exodus in the Bible.[1] Anthrax is also mentioned by Greek and Roman authors such as Homer (in The Iliad), Virgil (Georgics), and Hippocrates. Anthrax can also infect humans, usually as the result of coming into contact with infected animal hides, fur, wool ("Woolsorter's disease"), leather or contaminated soil. Anthrax ("siberian ulcer" [2]) is now fairly rare in humans, although it still regularly occurs in ruminants, such as cattle, sheep, goats, camels, wild buffalo, and antelopes, in hind-gut fermenters such as zebras and rhinos, and in other wildlife such as elephants and lions in certain endemic areas of the world.
Bacillus anthracis bacteria spores are soil-borne and because of their long lifetime, they are still present globally and at animal burial sites of anthrax-killed animals for many decades; spores have been known to have reinfected animals over 70 years after burial sites of anthrax-infected animals were disturbed. [3]
Until the twentieth century, anthrax infections killed hundreds and thousands of animals and people each year in Europe, Asia, Africa, Australia, and Southern Vietnam, specifically in the concentration camps during WWI, and North America.[4] French scientist Louis Pasteur developed the first effective vaccine for anthrax in 1881.[5][6][7] Thanks to over a century of animal vaccination programs, sterilization of raw animal waste materials and anthrax eradication programs in North America, Australia, New Zealand, Russia, Europe and parts of Africa and Asia, anthrax infection is now relatively rare in domestic animals with normally only a few dozen cases reported every year. Anthrax is even rarer in dogs and cats: there had only ever been one documented case in dogs in the USA by 2001, although the disease affects livestock.[8] Anthrax typically does not cause disease in carnivores and scavengers, even when these animals consume anthrax-infected carcasses. Anthrax outbreaks do occur in some wild animal populations with some regularity.[9] The disease is more common in developing countries without widespread veterinary or human public health programs.
There are 89 known strains of anthrax. The virulent Ames strain, which had been used in the 2001 anthrax attacks in the United States, has received the most news coverage of any anthrax outbreak. However, the Vollum strain, developed but never used as a biological weapon during the Second World War, is much more dangerous. The Vollum (also incorrectly referred to as Vellum) strain was isolated in 1935 from a cow in Oxfordshire, UK. This is the same strain that was used during the Gruinard bioweapons trials. A variation of Vollum known as "Vollum 1B" was used during the 1960s in the US and UK bioweapon programs. Vollum 1B was isolated from William A. Boyles, a 46-year-old USAMRIID scientist who died in 1951 after being accidentally infected with the Vollum strain. The Sterne strain, named after a South African researcher, is an attenuated strain used as a vaccine.
[edit] Description of the bacterium

Bacillus anthracis is a rod-shaped Gram-positive bacterium, about 1 by 9 micrometers in size. It was shown to cause disease by Robert Koch in 1877.[7] The bacterium normally rests in endospore form in the soil, and can survive for up to decades in this state. Herbivores are often infected whilst grazing or browsing, especially when eating rough, irritant or spiky vegetation: the vegetation has been hypothesized to cause wounds within the gastrointestinal tract permitting entry of the bacterial endo-spores into the tissues, though this has not been proven. Once ingested or placed in an open cut, the bacterium begins multiplying inside the animal or human and typically kills the host within a few days or weeks. The endo-spores germinate at the site of entry into the tissues and then spread via the circulation to the lymphatics, where the bacteria multiply. It is the production of two powerful exo-toxins (edema toxin and lethal toxin) by the bacteria that causes death. Veterinarians can often tell a possible anthrax-induced death by its sudden occurrence, and by the dark, non-clotting blood that oozes from the body orifices. Most anthrax bacteria inside the body after death are out-competed and destroyed by anaerobic bacteria within minutes to hours post-mortem. However, anthrax vegetative bacteria that escape the body via oozing blood or through the opening of the carcass may form hardy spores. One spore forms per one vegetative bacterium. The triggers for spore formation are not yet known, though oxygen tension and lack of nutrients may play roles. Once formed, these spores are very hard to eradicate.
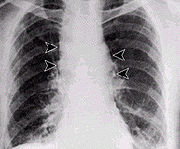
The infection of herbivores (and occasionally humans) via the inhalational route normally proceeds as follows: once the spores are inhaled, they are transported through the air passages into the tiny air sacs (alveoli) in the lungs. The spores are then picked up by scavenger cells (macrophages) in the lungs and are transported through small vessels (lymphatics) to the lymph nodes in the central chest cavity (mediastinum). Damage caused by the anthrax spores and bacilli to the central chest cavity can cause chest pain and difficulty breathing. Once in the lymph nodes, the spores germinate into active bacilli which multiply and eventually burst the macrophages, releasing many more bacilli into the bloodstream to be transferred to the entire body. Once in the blood stream these bacilli release three substances: lethal factor, oedema factor and protective antigen. Protective antigen combines with these other two factors to form lethal toxin and oedema toxin, respectively. These toxins are the primary agents of tissue destruction, bleeding, and death of the host. If antibiotics are administered too late, even if the antibiotics eradicate the bacteria, some hosts will still die. This is because the toxins produced by the bacilli remain in their system at lethal dose levels.
In order to enter the cells, the edema and lethal factors use another protein produced by B. anthracis, protective antigen. Oedema factor inactivates neutrophils (a type of phagocytic cell) so that they cannot phagocytose bacteria. Historically, it was believed that lethal factor caused macrophages to make TNF-alpha and interleukin 1, beta (IL1B), both normal components of the immune system used to induce an inflammatory reaction, ultimately leading to septic shock and death. However, recent evidence indicates that anthrax also targets endothelial cells (cells that lines serous cavities, lymph vessels, and blood vessels), causing vascular leakage of fluid and cells, and ultimately hypovolemic shock (low blood volume), and septic shock.
The virulence of a strain of anthrax is dependent on multiple factors, primarily the poly-D-glutamic acid capsule that protects the bacterium from phagocytosis by host neutrophils and its toxins, edema toxin and lethal toxin.
[edit] Exposure
Occupational exposure to infected animals or their products (such as skin wool and meat) is the usual pathway of exposure for humans. Workers who are exposed to dead animals and animal products are at the highest risk, especially in countries where anthrax is more common. Anthrax in livestock grazing on open range where they mix with wild animals still occasionally occurs in the United States and elsewhere. Many workers who deal with wool and animal hides are routinely exposed to low levels of anthrax spores but most exposures are not sufficient to develop anthrax infections. Presumably, the body’s natural defenses can destroy low levels of exposure. These people usually contract cutaneous anthrax if they catch anything. Historically, the most dangerous form of inhalational anthrax was called Woolsorters' disease because it was an occupational hazard for people who sorted wool. Today this form of infection is extremely rare, as almost no infected animals remain. The last fatal case of natural inhalational anthrax in the United States occurred in California in 1976, when a home weaver died after working with infected wool imported from Pakistan. The autopsy was done at UCLA hospital. To minimize the chance of spreading the disease, the deceased was transported to UCLA in a sealed plastic body bag within a sealed metal container.[10]
In November 2008, a drum maker in the United Kingdom who worked with untreated animal skins became the latest person to die from anthrax.[11]
[edit] Mode of infection
Anthrax can enter the human body through the intestines (ingestion), lungs (inhalation), or skin (cutaneous) and causes distinct clinical symptoms based on its site of entry. An infected human will generally be quarantined. However, anthrax does not usually spread from an infected human to a noninfected human. But if the disease is fatal the person’s body and its mass of anthrax bacilli becomes a potential source of infection to others and special precautions should be used to prevent further contamination. Inhalational anthrax, if left untreated until obvious symptoms occur, may be fatal.
Anthrax can be contracted in laboratory accidents or by handling infected animals or their wool or hides. It has also been used in biological warfare agents and by terrorists to intentionally infect humans, as occurred in, for example, the 2001 anthrax attacks.
[edit] Pulmonary (pneumonic, respiratory, or inhalational) anthrax
Respiratory infection in humans initially presents with cold or flu-like symptoms for several days, followed by severe (and often fatal) respiratory collapse. This disease can rarely be treated, even if caught in early stages of infection; mortality is nearly 100%.[12] A lethal infection is reported to result from inhalation of about 10,000–20,000 spores, though this dose varies amongst host species.[13] Like all diseases there is probably a wide variation to susceptibility with evidence that some people may die from much lower exposures; there is little documented evidence to verify the exact or average number of spores needed for infection. Inhalational anthrax is also known as woolsorters' or ragpickers' disease as these professions were more susceptible to the disease due to their exposure to infected animal products. Other practices associated with exposure include the slicing up of animal horns for the manufacture of buttons, the handling of hair bristles used for the manufacturing of brushes, and the handling of animal skins. Whether these animal skins came from animals that died of the disease or from animals that had simply laid on ground that had spores on it is unknown. This mode of infection is used as a bioweapon.
[edit] Gastrointestinal (gastroenteric) anthrax
Gastrointestinal infection in humans is most often caused by eating anthrax-infected meat and is characterized by serious gastrointestinal difficulty, vomiting of blood, severe diarrhea, acute inflammation of the intestinal tract, and loss of appetite. Some lesions have been found in the intestines and in the mouth and throat. After the bacteria invades the bowel system, it spreads through the bloodstream throughout the body, making even more toxins on the way. Gastrointestinal infections can be treated but usually result in fatality rates of 25% to 60%, depending upon how soon treatment commences. [14]
[edit] Cutaneous (skin) anthrax
Cutaneous (on the skin) anthrax infection in humans shows up as a boil-like skin lesion that eventually forms an ulcer with a black centre (eschar). The black eschar often shows up as a large, painless necrotic ulcer (beginning as an irritating and itchy skin lesion or blister that is dark and usually concentrated as a black dot, somewhat resembling bread mold) at the site of infection. Cutaneous infections generally form within the site of spore penetration between 2 and 5 days after exposure. Unlike bruises or most other lesions, cutaneous anthrax infections normally do not cause pain. [14]
Cutaneous anthrax is rarely fatal if treated[12], but without treatment about 20% of cutaneous skin infection cases progress to toxemia and death.
[edit] Treatment and prevention
Anthrax cannot be spread directly from person to person, but a patient’s clothing and body may be contaminated with anthrax spores. Effective decontamination of people can be accomplished by a thorough wash down with antimicrobial effective soap and water. Waste water should be treated with bleach or other anti-microbial agent. Effective decontamination of articles can be accomplished by boiling contaminated articles in water for 30 minutes or longer. Chlorine bleach is ineffective in destroying spores and vegetative cells on surfaces, though formaldehyde is effective. Burning clothing is very effective in destroying spores. After decontamination, there is no need to immunize, treat or isolate contacts of persons ill with anthrax unless they were also exposed to the same source of infection. Early antibiotic treatment of anthrax is essential—delay seriously lessens chances for survival. Treatment for anthrax infection and other bacterial infections includes large doses of intravenous and oral antibiotics, such as fluoroquinolones, like ciprofloxacin (cipro), doxycycline, erythromycin, vancomycin or penicillin. In possible cases of inhalation anthrax, early antibiotic prophylaxis treatment is crucial to prevent possible death. If death occurs from anthrax the body should be isolated to prevent possible spread of anthrax germs. Burial does not kill anthrax spores.
If a person is suspected as having died from anthrax, every precaution should be taken to avoid skin contact with the potentially contaminated body and fluids exuded through natural body openings. The body should be put in strict quarantine. A blood sample taken in a sealed container and analyzed in an approved lab should be used to ascertain if anthrax is the cause of death. Microscopic visualization of the encapsulated bacilli, usually in very large numbers, in a blood smear stained with polychrome methylene blue (McFadyean stain) is fully diagnostic, though culture of the organism is still the gold standard for diagnosis. Full isolation of the body is important to prevent possible contamination of others. Protective, impermeable clothing and equipment such as rubber gloves, rubber apron, and rubber boots with no perforations should be used when handling the body. No skin, especially if it has any wounds or scratches, should be exposed. Disposable personal protective equipment is preferable, but if not available, decontamination can be achieved by autoclaving. Disposable personal protective equipment and filters should be autoclaved, and/or burned and buried. Bacillus anthracis bacillii range from 0.5-5.0 μm in size. Anyone working with anthrax in a suspected or confirmed victim should wear respiratory equipment capable of filtering this size of particle or smaller. The US National Institute for Occupational Safety and Health (NIOSH) and Mine Safety and Health Administration (MSHA) approved high efficiency-respirator, such as a half-face disposable respirator with a high-efficiency particulate air (HEPA) filter, is recommended. All possibly contaminated bedding or clothing should be isolated in double plastic bags and treated as possible bio-hazard waste. The victim should be sealed in an airtight body bag. Dead victims that are opened and not burned provide an ideal source of anthrax spores. Cremating victims is the preferred way of handling body disposal. No embalming or autopsy should be attempted without a fully equipped biohazard lab and trained and knowledgeable personnel.
Delays of only a few days may make the disease untreatable and treatment should be started even without symptoms if possible contamination or exposure is suspected. Animals with anthrax often just die without any apparent symptoms. Initial symptoms may resemble a common cold – sore throat, mild fever, muscle aches and malaise. After a few days, the symptoms may progress to severe breathing problems and shock and ultimately death. Death can occur from about two days to a month after exposure with deaths apparently peaking at about 8 days after exposure. [15] Antibiotic-resistant strains of anthrax are known.
In recent years there have been many attempts to develop new drugs against anthrax, but existing drugs are effective if treatment is started soon enough.
Early detection of sources of anthrax infection can allow preventative measures to be taken. In response to the anthrax attacks of October, 2001 the United States Postal Service (USPS) installed BioDetection Systems (BDS) in their large scale mail cancellation facilities. BDS response plans were formulated by the USPS in conjunction with local responders including fire, police, hospitals and public health. Employees of these facilities have been educated about anthrax, response actions and prophylactic medication. Because of the time delay inherent in getting final verification that anthrax has been used, prophylactic antibiotic treatment of possibly exposed personnel must be started as soon as possible.
The most effective form of prevention is vaccination against infection but this must be done well in advance of exposure to the bacillus, and does not protect indefinitely.
Components of tea, such as polyphenols, have the ability to inhibit the activity both of bacillus anthracis and its toxin considerably; spores, however, are not affected. The addition of milk to the tea completely inhibits its antibacterial activity against anthrax[16]. Activity against the anthrax bacillum in the laboratory does not prove that drinking tea affects the course of an infection.
[edit] Anthrax vaccines
An FDA-licensed vaccine, produced from one non-virulent strain of the anthrax bacterium, is manufactured by BioPort Corporation, subsidiary of Emergent BioSolutions. The trade name is BioThrax, although it is commonly called Anthrax Vaccine Adsorbed (AVA). It is administered in a six-dose primary series at 0,2,4 weeks and 6,12,18 months; annual booster injections are required thereafter to maintain immunity. The injections are typically very painful, and may leave the area of injection with swelling; this area may be painful for several days.
Unlike the West, the Soviets developed and used a live spore anthrax vaccine, known as the STI vaccine, produced in Tbilisi, Georgia. Its serious side effects restrict use to healthy adults.[17]
[edit] Site cleanup
Anthrax spores can survive for long periods of time in the environment after release. Methods for cleaning anthrax-contaminated sites commonly use oxidizing agents such as peroxides, ethylene oxide, Sandia Foam,[18] chlorine dioxide (used in Hart Senate office building), and liquid bleach products containing sodium hypochlorite. These agents slowly destroy bacterial spores. A bleach solution for treating hard surfaces has been approved by the EPA.[19] It can be prepared by mixing one part bleach (5.25%-6.00%) to one part white vinegar to eight parts water. Bleach and vinegar must not be combined together directly, as doing so could produce chlorine gas. Rather some water must first be added to the bleach (e.g., two cups water to one cup of bleach), then vinegar (e.g., one cup), and then the rest of the water (e.g., six cups). The pH of the solution should be tested with a paper test strip; and treated surfaces must remain in contact with the bleach solution for 60 minutes (repeated applications will be necessary to keep the surfaces wet).
Chlorine dioxide has emerged as the preferred biocide against anthrax-contaminated sites, having been employed in the treatment of numerous government buildings over the past decade. Its chief drawback is the need for in situ processes to have the reactant on demand.
To speed the process, trace amounts of a non-toxic catalyst composed of iron and tetro-amido macrocyclic ligands are combined with sodium carbonate and bicarbonate and converted into a spray. The spray formula is applied to an infested area and is followed by another spray containing tertiary-butyl hydroperoxide.[citation needed]
Using the catalyst method, a complete destruction of all anthrax spores takes 30 minutes.[citation needed] A standard catalyst-free spray destroys fewer than half the spores in the same amount of time. They can be heated, exposed to the harshest chemicals, and they do not easily die.
Cleanups at a Senate office building, several contaminated postal facilities and other U.S. government and private office buildings showed that decontamination is possible, but it is time-consuming and costly. Clearing the Senate office building of anthrax spores cost $27 million, according to the Government Accountability Office. Cleaning the Brentwood postal facility outside Washington cost $130 million and took 26 months. Since then newer and less costly methods have been developed.[20]
Clean up of anthrax-contaminated areas on ranches and in the wild is much more problematic. Carcasses may be burned, though it often takes up to three days to burn a large carcass and this is not feasible in areas with little wood. Carcasses may be buried, though the burying of large animals deeply enough to prevent resurfacing of spores requires much manpower and expensive tools. Carcasses have been soaked in formaldehyde to kill spores, though this has obvious environmental contamination issues. Block burning of vegetation in large areas enclosing an anthrax outbreak has been tried; this, while environmentally destructive, causes healthy animals to move away from an area with carcasses in search of fresh graze and browse. Some wildlife workers have experimented with covering fresh anthrax carcasses with shadecloth and heavy objects. This prevents some scavengers from opening the carcasses, thus allowing the putrefactive bacteria within the carcass to kill the vegetative B. anthracis cells and preventing sporulation. This method also has drawbacks, as scavengers such as hyenas are capable of infiltrating almost any exclosure. The occurrence of previously dormant anthrax, stirred up from below the ground surface by wind movement in a drought-stricken region with depleted grazing and browsing, may be seen as a form of natural culling and a first step in rehabilitation of the area.
[edit] History
[edit] Discovery
Robert Koch, a German physician and scientist, first identified the bacteria which caused the anthrax disease in 1875.[21] His pioneering work in the late nineteenth century was one of the first demonstrations that diseases could be caused by microbes. In a groundbreaking series of experiments he uncovered the life cycle and means of transmission of anthrax. His experiments not only helped create an understanding of anthrax, but also helped elucidate the role of microbes in causing illness at a time when debates were still held over spontaneous generation versus cell theory. Koch went on to study the mechanisms of other diseases and was awarded the 1905 Nobel Prize in Physiology or Medicine for his discovery of the bacteria causing tuberculosis. Koch is today recognized as one of history's most important biologists and a founder of modern bacteriology.
[edit] First vaccination
In May 1881 Louis Pasteur performed a public experiment to demonstrate his concept of vaccination. He prepared two groups of 25 sheep, one goat and several cows. The animals of one group were injected with an anti-anthrax vaccine prepared by Pasteur twice, at an interval of 15 days; the control group was left unvaccinated. Thirty days after the first injection both groups were injected with a culture of live anthrax bacteria. All the animals in the non-vaccinated group died, while all of the animals in the vaccinated group survived.[22]
After mastering method of vaccination Pasteur applied the concept to rabies. He went on to develop vaccines against small pox, cholera, and swine erysipelas.
The human vaccine for anthrax became available in 1954. This was a cell-free vaccine instead of the live-cell Pasteur-style vaccine used for veterinary purposes. An improved cell-free vaccine became available in 1970.[23]
[edit] Biological warfare
"Anthrax was first tested as a biological warfare agent by Unit 731 of the Japanese Kwantung Army in Manchuria during the 1930s; some of this testing involved intentional infection of prisoners of war, thousands of whom died. Anthrax, designated at the time as Agent N, was also investigated by the allies in the 1940s. The British army tested experimental anthrax weapons on Gruinard Island, off the northwest coast of Scotland, in 1943. Gruinard was burned over at least once, yet as of the late 1980s, it was still too heavily contaminated with spores to allow unprotected human access, indicating the hardiness of anthrax spores. Weaponized anthrax was part of the U.S. stockpile prior to its destruction in 1972."

Anthrax spores can and have been used as a biological warfare weapon. Its first modern incidence occurred when Scandinavian "freedom fighters" (the rebel groups) supplied by the German General Staff used anthrax with unknown results against the Imperial Russian Army in Finland in 1916.[24] There is a long history of practical bioweapons research in this area. For example, in 1942 British bioweapons trials[25] severely contaminated Gruinard Island in Scotland with anthrax spores of the Vollum-14578 strain, making it a no-go area until it was decontaminated in 1990.[26] The Gruinard trials involved testing the effectiveness of a submunition of an "N-bomb"—a biological weapon. Additionally, five million "cattle cakes" impregnated with anthrax were prepared and stored at Porton Down in 'Operation Vegetarian'—an anti-livestock weapon intended for attacks on Germany by the Royal Air Force[27] The infected cattle cakes were to be dropped on Germany in 1944. However neither the cakes nor the bomb were used; the cattle cakes were incinerated in late 1945.
More recently the Rhodesian government used anthrax against cattle and humans in the period 1978–1979 during its war with black nationalists.[28]
American military and British Army personnel are routinely vaccinated against anthrax prior to active service in places where biological attacks are considered a threat. The anthrax vaccine, produced by BioPort Corporation, contains non-living bacteria, and is approximately 93% effective in preventing infection.[citation needed]
Weaponized stocks of anthrax in the US were destroyed in 1971–72 after President Nixon ordered the dismantling of US biowarfare programs in 1969 and the destruction of all existing stockpiles of bioweapons. Research is known to continue in the United States on ways to counteract bioweapons attacks.
The Soviet Union created and stored 100 to 200 tons of anthrax spores on Vozrozhdeniya Island. They were abandoned in 1992 and destroyed in 2002.
[edit] Soviet accident: April 2, 1979
Despite signing the 1972 agreement to end bioweapon production the government of the Soviet Union had an active bioweapons program that included the production of hundreds of tons of weapons-grade anthrax after this period. On April 2, 1979 some of the over one million people living in Sverdlovsk (now called Ekaterinburg, Russia), about 850 miles east of Moscow, were exposed to an accidental release of anthrax from a biological weapons complex located near there. At least 94 people were infected, of whom at least 68 died. One victim died four days after the release, ten over an eight-day period at the peak of the deaths, and the last six weeks later. Extensive cleanup, vaccinations and medical interventions managed to save about 30 of the victims. [29] Extensive cover-ups and destruction of records by the KGB continued from 1979 until Russian President Boris Yeltsin admitted this anthrax accident in 1992. Jeanne Guillemin reported in 1999 that a combined Russian and United States team investigated the accident in 1992.[30][31][32]
Nearly all of the night shift workers of a ceramics plant directly across the street from the biological facility (compound 19) became infected, and most died. Since most were men, there were suspicions by Western governments that the Soviet Union had developed a sex-specific weapon.[33] The government blamed the outbreak on the consumption of anthrax-tainted meat and ordered the confiscation of all uninspected meat that entered the city. They also ordered that all stray dogs be shot and that people not have contact with sick animals. There was also a voluntary evacuation and anthrax vaccination program established for people from 18–55.[34]
To support the cover-up story Soviet medical and legal journals published articles about an outbreak in livestock that caused GI anthrax in people who consumed infected meat, and cutaneous anthrax in people who came into contact with the animals. All medical and public health records were confiscated by the KGB.[34] In addition to the medical problems that the outbreak caused, it also prompted Western countries to be (justifiably) more suspicious of a covert Soviet Bioweapons program and to increase their surveillance of suspected sites. In 1986 the US government was allowed to investigate the incident, and concluded that the exposure was from aerosol anthrax from a military weapons facility.[35] In 1992, President Yeltsin admitted that he was "absolutely certain" that "rumors" about the Soviet Union violating the 1972 Bioweapons Treaty were true. The Soviet Union, like the US and UK, had agreed to submit information to the UN about their bioweapons programs but omitted known facilities and never acknowledged their weapons program.[33]
[edit] Anthrax bioterrorism
Theoretically anthrax spores can be cultivated with minimal special equipment and a first-year collegiate microbiological education, but in practice the procedure is difficult and dangerous. To make large amounts of an aerosol form of anthrax suitable for biological warfare, extensive practical knowledge, training and highly advanced equipment are required.
Concentrated anthrax spores were used for bioterrorism in the 2001 anthrax attacks in the United States, delivered by mailing postal letters containing the spores. Only a few grams of material were used in these attacks and in August 2008 the US Department of Justice announced they believed that Dr. Bruce Ivins, a senior biodefense researcher, was responsible. [36] These events also spawned many anthrax hoaxes.
Due to these events, the U.S. Postal Service installed biohazard detection systems at its major distribution centers to actively scan for anthrax being transported through the mail. [37]
[edit] Decontaminating mail
In response to the postal anthrax attacks and hoaxes the US Postal Service sterilized some mail using a process of gamma irradiation and treatment with a proprietary enzyme formula supplied by Sipco Industries Ltd.[38]
A scientific experiment performed by a high school student, later published in The Journal of Medical Toxicology, suggested that a domestic electric iron at its hottest setting (at least 400 °F (204 °C)) used for at least 5 minutes should destroy all anthrax spores in a common postal envelope.[39]
[edit] See also
- 2001 anthrax attacks
- Anthrax hoaxes
- Ames strain
- Gruinard Island - site of British bioweapons trials in 1942
- Sverdlovsk Anthrax leak
- Anthrax toxin
- Anthrax Detection Device
- Anthrax Vaccine
- Anthrax Vaccine Immunization Program, or AVIP: the program for vaccinating all members of the armed services in the United States.
- Black death
- Unit 731
[edit] References
- ^ Blanc, H. W. (1890). "Anthrax: the disease of the Egyptian plagues". New Orleans Med Surg J 18: 1–25.
- ^ Jeanne Guillemin. Anthrax. The Investigation of a Deadly Outbreak
- ^ "Anthrax" by Jeanne Guillemin, University of California Press, 2001, ISBN 0-520-22917-7, pg. 3
- ^ Cherkasskiy, B. L. (1999). "A national register of historic and contemporary anthrax foci". Journal of Applied Microbiology 87 (2): 192–195. doi:.
- ^ David V. Cohn (1996-02-11). "Life and Times of Louis Pasteur". School of Dentistry, University of Louisville. http://louisville.edu/library/ekstrom/special/pasteur/cohn.html. Retrieved on 2008-08-13.
- ^ Mikesell, P.; Ivins, B. E.; Ristroph, J. D.; Vodkin, M. H.; Dreier, T. M.; Leppla, S. H. (1983), "Plasmids, Pasteur, and Anthrax" (PDF), ASM News 49: 320–322, http://www.asm.org/ASM/files/CCLIBRARYFILES/FILENAME/0000000221/490783p320.pdf
- ^ a b "Robert Koch (1843-1910)". About.com. http://german.about.com/library/blerf_koch.htm. Retrieved on 2008-08-13.
- ^ "Can Dogs Get Anthrax?" Canine Nation, 30 October 2001. Retrieved 17 February 2007.
- ^ Dragon, D. C. (1999). "A review of anthrax in Canada and implications for research on the disease in northern bison". Journal of Applied Microbiology 87: 208. doi:.
- ^ Suffin, S. C.; Carnes, W. H.; Kaufmann, A. F. (September 1978). "Inhalation anthrax in a home craftsman". Human Pathology 9 (5): 594–597. http://www.ncbi.nlm.nih.gov/pubmed/101438.
- ^ "Man who breathed in anthrax dies," BBC News, 2 November 2008. Retrieved 2 November 2008.
- ^ a b Bravata DM, Holty JE, Liu H, McDonald KM, Olshen RA, Owens DK (2006), Systematic review: a century of inhalational anthrax cases from 1900 to 2005, Annals of Internal Medicine; 144(4): 270–80.
- ^ "Anthrax, Then and Now". MedicineNet.com. http://www.medicinenet.com/script/main/art.asp?articlekey=18812&page=2. Retrieved on 2008-08-13.
- ^ a b "Anthrax Q & A: Signs and Symptoms". Emergency Preparedness and Response. Centers for Disease Control and Prevention. 2003. http://www.bt.cdc.gov/agent/anthrax/faq/signs.asp. Retrieved on 2007-04-19.
- ^ ANTHRAX, the investigation of a Deadly Outbreak, Jeanne Guillemin, University of California Press, 1999, ISBN 0=520-22917-7, chart of Russian deaths at Sverdlovsk, 1979, pg 27
- ^ "Anthrax and tea". Society for Applied Microbiology. 2008-03-17. http://www.sfam.org.uk/newsarticle.php?214&2. Retrieved on 2008-08-13.
- ^ ANTHRAX, the investigation of a Deadly Outbreak, Jeanne Guillemin, University of California Press, 1999, ISBN 0=520-22917-7, pg 34
- ^ "Sandia decon formulation, best known as an anthrax killer, takes on household mold". 2007-04-26. http://www.eurekalert.org/pub_releases/2007-04/dnl-sdf042607.php. Retrieved on 2008-08-13.
- ^ "Using Bleach to Destroy Anthrax and Other Microbes". Society for Applied Microbiology. http://ehso.com/bleach.htm. Retrieved on 2008-08-13.
- ^ The Bulletin Vol. 57 - No. 36 October 17, 2003PDF (332 KiB)[verification needed]
- ^ Madigan M; Martinko J (editors). (2005). Brock Biology of Microorganisms (11th ed. ed.). Prentice Hall. ISBN 0-13-144329-1.
- ^ Decker, Janet. Deadly Diseases and Epidemics, Anthrax. Chelesa House Publishers, 2003. ISBN 0-7910-7302-5 p 27–28.
- ^ "Anthrax and Anthrax Vaccine - Epidemiology and Prevention of Vaccine-Preventable Diseases", National Immunization Program, Centers for Disease Control and Prevention, January 2006. (PPT format)
- ^ Bisher, Jamie, "During World War I, Terrorists Schemed to Use Anthrax in the Cause of Finnish Independence," Military History, August 2003, pp. 17-22. Anthrax Sabotage in Finland
- ^ [1]
- ^ "Saddam's germ war plot is traced back to one Oxford cow," The Times
- ^ "UK planned to wipe out Germany with anthrax". Sunday Herald (Glasgow). 2001-10-14. http://www.fpp.co.uk/bookchapters/WSC/Bwar2.html. Retrieved on 2008-08-13.
- ^ Southern African News Feature : the plague wars
- ^ ANTHRAX, the investigation of a Deadly Outbreak, Jeanne Guillemin, University of California Press, 1999, ISBN 0=520-22917-7, names of victims, pg 275-277
- ^ Guillmin, op. cit.
- ^ "Plague war: The 1979 anthrax leak". Frontline. PBS. http://www.pbs.org/wgbh/pages/frontline/shows/plague/sverdlovsk/. Retrieved on 2008-08-13.
- ^ Michael C. Fishbein. "Anthrax - From Russia with Love". Infectious Diseases: Causes, Types, Prevention, Treatment and Facts. MedicineNet.com. http://www.medicinenet.com/script/main/art.asp?articlekey=18982. Retrieved on 2008-08-13.
- ^ a b Alibek, K. Biohazard. New York, New York: Dell Publishing, 1999.
- ^ a b Meselson, M. et al (1994). "The Sverdlovsk Outbreak of 1979". Science 266(5188) 1202–1208
- ^ Sternbach, G. (2002). "The History of Anthrax". The Journal of Emergency Medicine 24(4) 463–467.
- ^ Bohn, Kevin (2008-08-06). "U.S. officials declare researcher is anthrax killer". CNN. http://www.cnn.com/2008/CRIME/08/06/anthrax.case/index.html. Retrieved on 2008-08-07.
- ^ "Cepheid, Northrop Grumman Enter Into Agreement for the Purchase of Anthrax Test Cartridges". Security Products. 2007-16-08. http://secprodonline.com/articles/2007/08/16/cepheid-northrop-grumman.aspx. Retrieved on 2009-26-03.
- ^ "Latest Facts Update". USPS. 2002-02-12. http://www.usps.com/news/facts/lfu_021202.htm. Retrieved on 2008-08-13.
- ^ "High school senior discovers ironing deactivates anthrax," Pittsburgh Tribune-Review, 20 February 2006
[edit] External links
| Wikinews has related news: 9/11 Anthrax investigation quietly loses urgency |
| Wikinews has related news: US Military To Buy Anthrax And Bioweapons Production Systems |
- Anthrax, Centers for Disease Control and Prevention (CDC)
- Anthrax factsheet from European Centre for Disease Prevention and Control, agency of European Union
- Agent Fact Sheet: Anthrax, Center for Biosecurity
- "Anthrax". CDC Division of Bacterial and Mycotic Diseases. http://www.cdc.gov/nczved/dfbmd/disease_listing/anthrax_gi.html. Retrieved on June 17.
- Bioterrorism Category A Agents - Information Resources
- "Bacillus anthracis and anthrax". Todar's Online Textbook of Bacteriology (University of Wisconsin-Madison Department of Bacteriology). http://textbookofbacteriology.net/Anthrax.html. Retrieved on June 17.
- "Focus on anthrax". Nature.com. http://www.nature.com/nature/anthrax/index.html. Retrieved on June 17.
- 2008 Ivins Court Documents and DOJ Report in convenient form.
|
||||||||||||||||||||



